The Burmese saying “တလိမ်နှစ်လိမ် ပွေလိမ်ရှုတ်” (ta-lain hna-lain pway-lain shoke) presents an intriguing exploration of complexity and fragility, particularly within the realms of psychology and nature. This metaphorical phrase, which translates roughly to “once twisted, twice twisted, entangled and broken,” serves as a poignant reminder of how intricate structures – be they biological, psychological, or emotional – are subject to both the beauty of their design and the perils of their entanglement.
The Burmese saying “တလိမ်နှစ်လိမ် ပွေလိမ်ရှုတ်” (ta-lain hna-lain pway-lain shoke) presents an intriguing exploration of complexity and fragility, particularly within the realms of psychology and nature. This metaphorical phrase, which translates roughly to “once twisted, twice twisted, entangled and broken,” serves as a poignant reminder of how intricate structures – be they biological, psychological, or emotional – are subject to both the beauty of their design and the perils of their entanglement. The wisdom embedded in this saying can be applied to the understanding of human nature, particularly in how we process experiences and how our biological makeup, exemplified by DNA, can reflect our psychological intricacies.
Complexity Through Twists
First and foremost, the concept of “twists” encapsulates the inherent complexity of both DNA and the human mind. The double helix of DNA exemplifies the beauty of molecular architecture, where each twist and turn is integral to its function. This spiral shape does not merely facilitate storage; it is a symbol of the intricate coding and regulatory mechanisms that govern life itself. Similarly, human cognition operates on multiple levels – thoughts, memories, and emotions intermingle and twist around one another, often leading to cognitive distortions. These distortions, such as overgeneralization or black-and-white thinking, represent the psychological equivalents of twisted strands of DNA.
When individuals encounter emotional challenges, their cognitive processes may become “twisted,” leading to an inaccurate perception of reality. Such cognitive distortions can cause significant distress, much like a malfunctioning DNA strand can lead to cellular abnormalities. In both scenarios, the organization of information is compromised, rendering the psychological ‘cell’ unable to function optimally. This comparison vividly illustrates that both the intricacies of our biological makeup and the processes of our mind can become ensnared in complexity, with dire consequences for our well-being.
Entanglement Leading to Fragility
The second part of the saying intimates that excessive twisting ultimately leads to rupture – an idea that resonates strongly with both psychological entanglement and genetic integrity. In psychology, individuals often experience a range of emotional tensions that, when unexamined or unresolved, create mental “knots” of distress. Overthinking, rumination, and suppressed emotions can manifest as anxiety, depression, or burnout. Much like a twist in a strand of DNA that increases the risk of mutations, a psychological “twist” can lead to a breakdown in mental health.
Daniel Kahneman’s work on cognitive biases illustrates how these psychological entanglements can distort decision-making and emotional responses. Over time, the failure to address or “untwist” these cognitive barriers can lead to a severe rupture in personal resilience and mental health, mirroring the catastrophic implications of a genetic mutation on health. In both fields, the fragility of these systems – whether they be biological or psychological – demands attention; without intervention, the outcomes can be devastating.
Nature’s Imperfect Beauty
Finally, the notion of imperfect beauty is a theme that resonates strongly within nature and human psychology alike. Nature, in its complexity and variety, embodies both harmony and error. DNA sequences, while primarily stable, can undergo mutations that lead to both advantageous traits and detrimental disorders. Similarly, the human psyche is often a tapestry of experiences, memories, and emotions that shape our identity. These experiences may be intentionally gathered or involuntarily twisted; both contribute to our understanding of self and our interactions with the world.
Psychotherapy can be likened to the scientific work of gene therapy – both aim to understand and repair what has gone awry. Cognitive Behavioural Therapy (CBT), for instance, seeks to untangle distorted thinking and reframe perspectives, much like scientific approaches that aim to correct genetic malfunctions. The objective in both instances is restoration and alignment, acknowledging the essential truth that while complexities exist, they can be navigated and repaired. This interplay between nature and psychology illustrates a fundamental truth: our lives are marked by an elegant, yet precarious, intertwining of structures at both micro and macro levels.
Conclusion
In conclusion, the Burmese saying “တလိမ်နှစ်လိမ် ပွေလိမ်ရှုတ်” (ta-lain hna-lain pway-lain shoke) encapsulates a profound truth about the complexity, entanglement, and fragility of life’s structures. Whether considering the molecular architecture of DNA or the intricacies of human psychology, the consequences of excessive twisting are clear. Both realms highlight the necessity of understanding and addressing the inherent complexities to prevent rupture and to promote healing and resilience. Life, with all its beautifully woven threads, invites us to engage with its challenges thoughtfully and intentionally, lest we succumb to chaos. Through such understanding and action, we can strive toward a state of balance – material, mental, and emotional.
The Burmese saying “တလိမ်နှစ်လိမ် ပွေလိမ်ရှုတ်” (ta-lain hna-lain pway-lain shoke) presents an intriguing exploration of complexity and fragility, particularly within the realms of psychology and nature. This metaphorical phrase, which translates roughly to “once twisted, twice twisted, entangled and broken,” serves as a poignant reminder of how intricate structures – be they biological, psychological, or emotional – are subject to both the beauty of their design and the perils of their entanglement. The wisdom embedded in this saying can be applied to the understanding of human nature, particularly in how we process experiences and how our biological makeup, exemplified by DNA, can reflect our psychological intricacies.
Complexity Through Twists
First and foremost, the concept of “twists” encapsulates the inherent complexity of both DNA and the human mind. The double helix of DNA exemplifies the beauty of molecular architecture, where each twist and turn is integral to its function. This spiral shape does not merely facilitate storage; it is a symbol of the intricate coding and regulatory mechanisms that govern life itself. Similarly, human cognition operates on multiple levels – thoughts, memories, and emotions intermingle and twist around one another, often leading to cognitive distortions. These distortions, such as overgeneralization or black-and-white thinking, represent the psychological equivalents of twisted strands of DNA.
When individuals encounter emotional challenges, their cognitive processes may become “twisted,” leading to an inaccurate perception of reality. Such cognitive distortions can cause significant distress, much like a malfunctioning DNA strand can lead to cellular abnormalities. In both scenarios, the organization of information is compromised, rendering the psychological ‘cell’ unable to function optimally. This comparison vividly illustrates that both the intricacies of our biological makeup and the processes of our mind can become ensnared in complexity, with dire consequences for our well-being.
Entanglement Leading to Fragility
The second part of the saying intimates that excessive twisting ultimately leads to rupture – an idea that resonates strongly with both psychological entanglement and genetic integrity. In psychology, individuals often experience a range of emotional tensions that, when unexamined or unresolved, create mental “knots” of distress. Overthinking, rumination, and suppressed emotions can manifest as anxiety, depression, or burnout. Much like a twist in a strand of DNA that increases the risk of mutations, a psychological “twist” can lead to a breakdown in mental health.
Daniel Kahneman’s work on cognitive biases illustrates how these psychological entanglements can distort decision-making and emotional responses. Over time, the failure to address or “untwist” these cognitive barriers can lead to a severe rupture in personal resilience and mental health, mirroring the catastrophic implications of a genetic mutation on health. In both fields, the fragility of these systems – whether they be biological or psychological – demands attention; without intervention, the outcomes can be devastating.
Nature’s Imperfect Beauty
Finally, the notion of imperfect beauty is a theme that resonates strongly within nature and human psychology alike. Nature, in its complexity and variety, embodies both harmony and error. DNA sequences, while primarily stable, can undergo mutations that lead to both advantageous traits and detrimental disorders. Similarly, the human psyche is often a tapestry of experiences, memories, and emotions that shape our identity. These experiences may be intentionally gathered or involuntarily twisted; both contribute to our understanding of self and our interactions with the world.
Psychotherapy can be likened to the scientific work of gene therapy – both aim to understand and repair what has gone awry. Cognitive Behavioural Therapy (CBT), for instance, seeks to untangle distorted thinking and reframe perspectives, much like scientific approaches that aim to correct genetic malfunctions. The objective in both instances is restoration and alignment, acknowledging the essential truth that while complexities exist, they can be navigated and repaired. This interplay between nature and psychology illustrates a fundamental truth: our lives are marked by an elegant, yet precarious, intertwining of structures at both micro and macro levels.
Conclusion
In conclusion, the Burmese saying “တလိမ်နှစ်လိမ် ပွေလိမ်ရှုတ်” (ta-lain hna-lain pway-lain shoke) encapsulates a profound truth about the complexity, entanglement, and fragility of life’s structures. Whether considering the molecular architecture of DNA or the intricacies of human psychology, the consequences of excessive twisting are clear. Both realms highlight the necessity of understanding and addressing the inherent complexities to prevent rupture and to promote healing and resilience. Life, with all its beautifully woven threads, invites us to engage with its challenges thoughtfully and intentionally, lest we succumb to chaos. Through such understanding and action, we can strive toward a state of balance – material, mental, and emotional.

In the gleaming, sterile halls of the Tokyo Spine Institute, where the hum of cutting-edge technology intertwines with the quiet intensity of scientific discovery, Dr Hiroshi Tanaka stands as a renegade in the world of pain management. With a glint of defiance in his eyes and a mind that refuses to bow to conventional wisdom, this renowned Japanese pain specialist has uncovered a truth so startling it’s sent shockwaves through the medical community. The culprit?
In the gleaming, sterile halls of the Tokyo Spine Institute, where the hum of cutting-edge technology intertwines with the quiet intensity of scientific discovery, Dr Hiroshi Tanaka stands as a renegade in the world of pain management. With a glint of defiance in his eyes and a mind that refuses to bow to conventional wisdom, this renowned Japanese pain specialist has uncovered a truth so startling it’s sent shockwaves through the medical community. The culprit? That seemingly innocent pillow on your bed, silently orchestrating a cascade of physical and neurological devastation while you sleep.
Dr Tanaka isn’t your typical doctor. There’s a spark of rebellion in his approach, a refusal to let the status quo go unchallenged. Using advanced muscle monitoring technology, he peered into the hidden world of sleep and discovered something chilling: your trapezius muscle — the crucial connector between your neck and shoulders — never gets a chance to rest. “It’s like torture for your body,” he declares, his voice a potent mix of urgency and exasperation. “Think about it; you’d never stand with your neck twisted for eight hours during the day. But that’s exactly what your regular pillow does to you every night.”
This alarming revelation explains why so many wake up to a litany of woes: neck pain that worsens with each passing day, headaches that cling like unwelcome guests, and sleep that feels less refreshing no matter how many hours you clock. Expensive treatments, from chiropractic sessions to painkillers, offer only fleeting relief, leaving patients trapped in a cycle of discomfort. According to Dr Tanaka’s research, this is merely the tip of the iceberg, a prelude to a far more sinister chain reaction.
The Pain Cascade Effect
Dr Tanaka’s research unveiled what he calls the “Pain Cascade Effect”, a term that carries the weight of a medical thriller. “What starts in your neck is just the beginning,” he warns, his tone laced with the gravity of someone who’s seen the evidence firsthand. The process is as insidious as it is relentless. While you sleep, your neck muscles lock up, taut as a rubber band stretched to its limit. This tension doesn’t stay confined; it spreads like wildfire into your shoulders, then creeps down into your upper back, weaving a web of pain that’s nearly impossible to untangle.
Using specialized blood flow imaging, Tanaka’s team uncovered something even more frightening: this constant muscle tension chokes off vital blood supply to these areas. “It’s like your body is slowly suffocating these muscles every single night,” he explains, painting a vivid picture of a body under siege. The result is a vicious cycle that compounds over time:
Chronic pain deepens, becoming a constant companion.
Muscles grow increasingly fatigued, robbed of the oxygen and nutrients they need.
Daily discomfort becomes the new normal, an accepted part of life.
The upper body ages prematurely, as if time itself is conspiring against you.
“Most disturbing,” Tanaka adds, his voice tinged with frustration, “is that traditional treatments can’t stop this cascade. As long as you’re using a regular pillow, you’re resetting this damage cycle every single night.” It’s a sobering thought — one that transforms the humble pillow from a symbol of rest into a silent saboteur.
A Neurological Nightmare Unfolds
But the stakes of Tanaka’s discovery climb even higher. His 25-year study at the Tokyo Spine Institute revealed a pattern that chilled even his seasoned colleagues: those unassuming pillows aren’t just causing physical pain; they’re triggering what he calls a “neurological nightmare.” The wrong pillow, it turns out, doesn’t merely strain muscles; it can spark severe neurological events, with migraines at the forefront.
“What we discovered about migraines was the most frightening part of our research,” Tanaka says, his voice growing sombre. These aren’t just ordinary headaches but debilitating migraines that bring dizziness, blurred vision, and nausea that can knock you off your feet. His findings point to a grim checklist of warning signs:
Headaches that strike without warning, like lightning from a clear sky.
Random bouts of dizziness that throw you off balance.
Strange spots or flashes in your vision, as if reality itself is glitching.
Nausea that leaves you reeling for no apparent reason.
Sudden sensitivity to light, forcing you to squint at sources that never bothered you before.
These symptoms, Tanaka argues, are the body’s desperate cry for help, a signal that the constant strain from improper pillow support is pushing the nervous system to its breaking point. The implications are staggering: something as simple as a pillow could be the hidden trigger behind debilitating neurological issues.
A Rebel with a Cause
What makes Dr Tanaka’s work so compelling isn’t just the science; it’s the man himself. There’s a fire in his words, a sense that he’s not merely uncovering facts but waging a war against a silent epidemic. His colleagues at the Tokyo Spine Institute describe him as a maverick, a doctor who combines rigorous methodology with an almost poetic passion for his patients’ well-being. “But here’s what makes my blood boil,” he says, his voice crackling with righteous anger, “the medical industry is making a fortune from your suffering.”
Tanaka’s accusation is bold, delivered with the conviction of a man who’s seen too many patients trapped in a cycle of temporary fixes — painkillers, physical therapy, and invasive procedures that fail to address the root cause. He points to a multi-billion-dollar industry that thrives on treating symptoms while ignoring the everyday culprits, like poorly designed pillows, that perpetuate the problem. It’s a system, he argues, that profits from keeping patients in pain rather than empowering them to break free.
His research paints a vivid picture of the stakes. Beyond the immediate discomfort, sleeping on the wrong pillow accelerates the ageing of your upper body, leaving muscles and joints worn out before their time. The chronic tension and restricted blood flow create a feedback loop that’s hard to escape, turning restful sleep into a nightly battle. And the neurological risks – those migraines and dizzy spells – add a layer of urgency that’s impossible to ignore.
The Pillow Revolution Begins
Dr Tanaka’s work is more than a scientific breakthrough; it’s a call to arms. In his lab, surrounded by the soft glow of monitors and the hum of progress, he’s peeling back the curtain on a health crisis hiding in plain sight. There’s something almost cinematic about his mission – a lone doctor taking on the Goliath of conventional medicine with nothing but data, determination, and a vision for change.
The implications of his findings are as practical as they are profound. That ordinary pillow, the one you’ve trusted for years, might be the key to unlocking a healthier, pain-free life — or the anchor dragging you deeper into discomfort. Tanaka’s research suggests that the solution lies in rethinking how we support our bodies during sleep, prioritizing pillows that alleviate tension rather than create it. It’s a simple fix with the potential to rewrite the health outcomes of millions.
As he stands at the forefront of this pillow revolution, Dr Tanaka embodies the spirit of a true innovator. His work challenges us to question the everyday objects we take for granted and to demand better for our bodies. There’s a quiet heroism in his persistence, a sense that he’s not just fighting for better sleep but for a world where pain doesn’t dictate our days. And as you lay your head down tonight, his warning lingers: the key to your health might just lie in the pillow you choose.
GNLM
In the gleaming, sterile halls of the Tokyo Spine Institute, where the hum of cutting-edge technology intertwines with the quiet intensity of scientific discovery, Dr Hiroshi Tanaka stands as a renegade in the world of pain management. With a glint of defiance in his eyes and a mind that refuses to bow to conventional wisdom, this renowned Japanese pain specialist has uncovered a truth so startling it’s sent shockwaves through the medical community. The culprit? That seemingly innocent pillow on your bed, silently orchestrating a cascade of physical and neurological devastation while you sleep.
Dr Tanaka isn’t your typical doctor. There’s a spark of rebellion in his approach, a refusal to let the status quo go unchallenged. Using advanced muscle monitoring technology, he peered into the hidden world of sleep and discovered something chilling: your trapezius muscle — the crucial connector between your neck and shoulders — never gets a chance to rest. “It’s like torture for your body,” he declares, his voice a potent mix of urgency and exasperation. “Think about it; you’d never stand with your neck twisted for eight hours during the day. But that’s exactly what your regular pillow does to you every night.”
This alarming revelation explains why so many wake up to a litany of woes: neck pain that worsens with each passing day, headaches that cling like unwelcome guests, and sleep that feels less refreshing no matter how many hours you clock. Expensive treatments, from chiropractic sessions to painkillers, offer only fleeting relief, leaving patients trapped in a cycle of discomfort. According to Dr Tanaka’s research, this is merely the tip of the iceberg, a prelude to a far more sinister chain reaction.
The Pain Cascade Effect
Dr Tanaka’s research unveiled what he calls the “Pain Cascade Effect”, a term that carries the weight of a medical thriller. “What starts in your neck is just the beginning,” he warns, his tone laced with the gravity of someone who’s seen the evidence firsthand. The process is as insidious as it is relentless. While you sleep, your neck muscles lock up, taut as a rubber band stretched to its limit. This tension doesn’t stay confined; it spreads like wildfire into your shoulders, then creeps down into your upper back, weaving a web of pain that’s nearly impossible to untangle.
Using specialized blood flow imaging, Tanaka’s team uncovered something even more frightening: this constant muscle tension chokes off vital blood supply to these areas. “It’s like your body is slowly suffocating these muscles every single night,” he explains, painting a vivid picture of a body under siege. The result is a vicious cycle that compounds over time:
Chronic pain deepens, becoming a constant companion.
Muscles grow increasingly fatigued, robbed of the oxygen and nutrients they need.
Daily discomfort becomes the new normal, an accepted part of life.
The upper body ages prematurely, as if time itself is conspiring against you.
“Most disturbing,” Tanaka adds, his voice tinged with frustration, “is that traditional treatments can’t stop this cascade. As long as you’re using a regular pillow, you’re resetting this damage cycle every single night.” It’s a sobering thought — one that transforms the humble pillow from a symbol of rest into a silent saboteur.
A Neurological Nightmare Unfolds
But the stakes of Tanaka’s discovery climb even higher. His 25-year study at the Tokyo Spine Institute revealed a pattern that chilled even his seasoned colleagues: those unassuming pillows aren’t just causing physical pain; they’re triggering what he calls a “neurological nightmare.” The wrong pillow, it turns out, doesn’t merely strain muscles; it can spark severe neurological events, with migraines at the forefront.
“What we discovered about migraines was the most frightening part of our research,” Tanaka says, his voice growing sombre. These aren’t just ordinary headaches but debilitating migraines that bring dizziness, blurred vision, and nausea that can knock you off your feet. His findings point to a grim checklist of warning signs:
Headaches that strike without warning, like lightning from a clear sky.
Random bouts of dizziness that throw you off balance.
Strange spots or flashes in your vision, as if reality itself is glitching.
Nausea that leaves you reeling for no apparent reason.
Sudden sensitivity to light, forcing you to squint at sources that never bothered you before.
These symptoms, Tanaka argues, are the body’s desperate cry for help, a signal that the constant strain from improper pillow support is pushing the nervous system to its breaking point. The implications are staggering: something as simple as a pillow could be the hidden trigger behind debilitating neurological issues.
A Rebel with a Cause
What makes Dr Tanaka’s work so compelling isn’t just the science; it’s the man himself. There’s a fire in his words, a sense that he’s not merely uncovering facts but waging a war against a silent epidemic. His colleagues at the Tokyo Spine Institute describe him as a maverick, a doctor who combines rigorous methodology with an almost poetic passion for his patients’ well-being. “But here’s what makes my blood boil,” he says, his voice crackling with righteous anger, “the medical industry is making a fortune from your suffering.”
Tanaka’s accusation is bold, delivered with the conviction of a man who’s seen too many patients trapped in a cycle of temporary fixes — painkillers, physical therapy, and invasive procedures that fail to address the root cause. He points to a multi-billion-dollar industry that thrives on treating symptoms while ignoring the everyday culprits, like poorly designed pillows, that perpetuate the problem. It’s a system, he argues, that profits from keeping patients in pain rather than empowering them to break free.
His research paints a vivid picture of the stakes. Beyond the immediate discomfort, sleeping on the wrong pillow accelerates the ageing of your upper body, leaving muscles and joints worn out before their time. The chronic tension and restricted blood flow create a feedback loop that’s hard to escape, turning restful sleep into a nightly battle. And the neurological risks – those migraines and dizzy spells – add a layer of urgency that’s impossible to ignore.
The Pillow Revolution Begins
Dr Tanaka’s work is more than a scientific breakthrough; it’s a call to arms. In his lab, surrounded by the soft glow of monitors and the hum of progress, he’s peeling back the curtain on a health crisis hiding in plain sight. There’s something almost cinematic about his mission – a lone doctor taking on the Goliath of conventional medicine with nothing but data, determination, and a vision for change.
The implications of his findings are as practical as they are profound. That ordinary pillow, the one you’ve trusted for years, might be the key to unlocking a healthier, pain-free life — or the anchor dragging you deeper into discomfort. Tanaka’s research suggests that the solution lies in rethinking how we support our bodies during sleep, prioritizing pillows that alleviate tension rather than create it. It’s a simple fix with the potential to rewrite the health outcomes of millions.
As he stands at the forefront of this pillow revolution, Dr Tanaka embodies the spirit of a true innovator. His work challenges us to question the everyday objects we take for granted and to demand better for our bodies. There’s a quiet heroism in his persistence, a sense that he’s not just fighting for better sleep but for a world where pain doesn’t dictate our days. And as you lay your head down tonight, his warning lingers: the key to your health might just lie in the pillow you choose.
GNLM

On 18 July 2025, the Ministry of Health officially appointed newly graduated doctors and dental surgeons as government gazetted officers. The ceremony of appointment was held at the Myanmar Convention Centre, Yangon. This day is not only a moment of renewal for the Ministry of Health, but also a highly significant milestone for the country and its people. It marks the day when the torch of compassion, responsibility, and scientific proficiency was passed on to the capable hands of a new generation of medical doctors and dental surgeons.
On 18 July 2025, the Ministry of Health officially appointed newly graduated doctors and dental surgeons as government gazetted officers. The ceremony of appointment was held at the Myanmar Convention Centre, Yangon. This day is not only a moment of renewal for the Ministry of Health, but also a highly significant milestone for the country and its people. It marks the day when the torch of compassion, responsibility, and scientific proficiency was passed on to the capable hands of a new generation of medical doctors and dental surgeons. It is a great success for our nation toward a healthy and strong society.
I would like to honour these new doctors as “heroes.” A doctor is someone who can sometimes cure, often relieve, but always must be able to comfort. The Art of Being a Doctor is fundamentally about the ability to comfort. Being a doctor is more than just a title. Doctors are guardians of life, relievers of pain, and symbols of hope for those who suffer.
Since independence, the Ministry of Health has been striving to enhance public health services, from urban hospitals to rural clinics. Generations of doctors have continued to serve with compassion and resilience despite facing numerous hardships. Today, that responsibility has been entrusted to our new doctors, who now step into the healthcare history of Myanmar to write its next chapter. Their road ahead will not always be smooth. There will be sleepless nights, moments of self-doubt, and times when the heavy responsibilities feel overwhelming. But the true measure of a person’s worth is not how they fare in comfort and ease, but how they stand and persevere through hardship and challenges. We all firmly believe that these new doctors will stand strong with integrity, grow with honesty, and lead with compassion.
Wearing the white duty coat is not merely putting on a uniform – it is a commitment. It is a promise to treat everyone with dignity and kindness; to uphold scientific integrity and ethical standards even in unseen moments; and to continue learning humbly and serve devotedly. The nation and its people are relying on them and placing trust and hope in them. So, know that as new doctors, you are not walking this journey alone – you are walking it with your country and its people.
To support the development of these new doctors, the government has been providing advanced training, international collaborations, and modern medical equipment. From 2021 until now, 318 postgraduate students have been sent abroad for further study, and 1,957 participants have been able to attend international conferences and seminars.
It is also important to acknowledge that, following the political events of 2021 and other circumstances, many healthcare workers left public hospitals, leaving the health system under significant strain. In response, the Ministry of Health has worked diligently to ensure that newly graduated doctors can promptly enter the workforce. These efforts have involved various strategies to urgently fill critical gaps in public healthcare delivery.
To make sure that the public receives the best possible healthcare, the Ministry of Health is working to follow the guidance of the Head of State, who said, “Every public hospital must have a doctor.” We can see that this plan is being put into action.
Doctors who became civil servants in previous years are now being transferred to smaller public hospitals in townships after gaining proper medical experience. These doctors are helping fill important gaps in healthcare services, and we are proud and happy to see their contribution.
At the same time, the government is showing appreciation for the work of healthcare workers. It is helping doctors by building more staff housing and providing support like special allowances, so they can work smoothly and comfortably. Overall, this is a joint effort. When our doctors become stronger and more capable, it is also a success for the country and its people.
A country’s development is not measured by wealth or weapons, but by the health, education, and happiness of its people. That’s why the service of new doctors is part of building the nation. With their own hands, they are helping shape the future of the country.
In conclusion, as new doctors start their journey – whether in big city hospitals or village clinics – they will play an important part in helping the country grow. It is hoped that they will keep a kind heart, grow stronger in their skills, and always remember their duty. The white coat they wear should stand for respect and care, not pride. And in difficult times, they may become a light for others, bringing comfort and healing to those who need it most.
On 18 July 2025, the Ministry of Health officially appointed newly graduated doctors and dental surgeons as government gazetted officers. The ceremony of appointment was held at the Myanmar Convention Centre, Yangon. This day is not only a moment of renewal for the Ministry of Health, but also a highly significant milestone for the country and its people. It marks the day when the torch of compassion, responsibility, and scientific proficiency was passed on to the capable hands of a new generation of medical doctors and dental surgeons. It is a great success for our nation toward a healthy and strong society.
I would like to honour these new doctors as “heroes.” A doctor is someone who can sometimes cure, often relieve, but always must be able to comfort. The Art of Being a Doctor is fundamentally about the ability to comfort. Being a doctor is more than just a title. Doctors are guardians of life, relievers of pain, and symbols of hope for those who suffer.
Since independence, the Ministry of Health has been striving to enhance public health services, from urban hospitals to rural clinics. Generations of doctors have continued to serve with compassion and resilience despite facing numerous hardships. Today, that responsibility has been entrusted to our new doctors, who now step into the healthcare history of Myanmar to write its next chapter. Their road ahead will not always be smooth. There will be sleepless nights, moments of self-doubt, and times when the heavy responsibilities feel overwhelming. But the true measure of a person’s worth is not how they fare in comfort and ease, but how they stand and persevere through hardship and challenges. We all firmly believe that these new doctors will stand strong with integrity, grow with honesty, and lead with compassion.
Wearing the white duty coat is not merely putting on a uniform – it is a commitment. It is a promise to treat everyone with dignity and kindness; to uphold scientific integrity and ethical standards even in unseen moments; and to continue learning humbly and serve devotedly. The nation and its people are relying on them and placing trust and hope in them. So, know that as new doctors, you are not walking this journey alone – you are walking it with your country and its people.
To support the development of these new doctors, the government has been providing advanced training, international collaborations, and modern medical equipment. From 2021 until now, 318 postgraduate students have been sent abroad for further study, and 1,957 participants have been able to attend international conferences and seminars.
It is also important to acknowledge that, following the political events of 2021 and other circumstances, many healthcare workers left public hospitals, leaving the health system under significant strain. In response, the Ministry of Health has worked diligently to ensure that newly graduated doctors can promptly enter the workforce. These efforts have involved various strategies to urgently fill critical gaps in public healthcare delivery.
To make sure that the public receives the best possible healthcare, the Ministry of Health is working to follow the guidance of the Head of State, who said, “Every public hospital must have a doctor.” We can see that this plan is being put into action.
Doctors who became civil servants in previous years are now being transferred to smaller public hospitals in townships after gaining proper medical experience. These doctors are helping fill important gaps in healthcare services, and we are proud and happy to see their contribution.
At the same time, the government is showing appreciation for the work of healthcare workers. It is helping doctors by building more staff housing and providing support like special allowances, so they can work smoothly and comfortably. Overall, this is a joint effort. When our doctors become stronger and more capable, it is also a success for the country and its people.
A country’s development is not measured by wealth or weapons, but by the health, education, and happiness of its people. That’s why the service of new doctors is part of building the nation. With their own hands, they are helping shape the future of the country.
In conclusion, as new doctors start their journey – whether in big city hospitals or village clinics – they will play an important part in helping the country grow. It is hoped that they will keep a kind heart, grow stronger in their skills, and always remember their duty. The white coat they wear should stand for respect and care, not pride. And in difficult times, they may become a light for others, bringing comfort and healing to those who need it most.

Emotional suffering is not merely a fleeting mood or psychological abstraction – it is deeply rooted in our neurobiology. The human brain carries the imprint of past pain within its very circuits, shaping how we perceive the world, regulate emotions, and relate to others.
Emotional suffering is not merely a fleeting mood or psychological abstraction – it is deeply rooted in our neurobiology. The human brain carries the imprint of past pain within its very circuits, shaping how we perceive the world, regulate emotions, and relate to others.
Eckhart Tolle’s concept of the “pain-body” – a reservoir of accumulated emotional pain – finds striking parallels in neuroscience. In particular, the brain’s limbic system, including the amygdala and hippocampus, encodes emotionally charged experiences. These memories are tagged as significant and can be reactivated by seemingly minor cues, often without conscious awareness. Far from fading over time, these emotional imprints are reinforced through repetition, forming feedback loops that keep old wounds alive in the present.
The pain-body, then, can be understood as a neuro-affective pattern, a system of heightened reactivity that feeds on attention, identification, and the constant replaying of personal narratives. When it is activated, we often feel hijacked: our bodies tense, our minds narrow, and we may behave in ways that feel impulsive or out of character. This happens because the prefrontal cortex, the part of the brain responsible for thoughtful decision-making, becomes inhibited, allowing the emotional brain to take control.
The key to dissolving the pain-body lies in disrupting these loops. Neuroscience points to the role of the anterior cingulate cortex, which governs attention. By cultivating present-moment awareness, we engage in what’s known as “top-down modulation” – the intentional use of higher brain functions to regulate emotional responses. This is not passive mindfulness, but active engagement: paying close attention to the raw sensation of emotion, rather than being swept away by the story we tell about it.
The pain-body is nourished by rumination, projection, and emotional fusion. Feeding it strengthens the brain’s synaptic pathways, making emotional reactivity a default state. Over time, suffering becomes a form of identity. To reverse this, we must learn to be still, not as a form of escape, but as a recalibration of the nervous system. Stillness allows us to step out of the cycle, to feel without becoming fused with what is felt.
True transformation doesn’t come from suppression or struggle. It comes from witnessing. In this act of gentle observation, we cease to feed the pain-body. Without attention, it begins to lose its grip. Compassion and presence become the dominant neural patterns. What emerges is not a life without pain, but a self no longer defined by it.
Let the pain-body starve. Let it shrink without your attention. As its voice fades, may you find a quieter mind, a clearer heart, and a presence grounded not in past suffering, but in the freedom to choose anew.
Why Old Hurts Still Echo – and How to Quiet Them
Painful memories aren’t just “in your head”. They live in your brain’s wiring, waiting for the right moment to flare up. This idea, popularized by writer Eckhart Tolle as the “pain-body,” lines up neatly with what neuroscientists see under the microscope.
How pain gets stored
• The limbic system – especially two almond-sized hubs called the amygdala and hippocampus – tags emotional events as important.
• Each time a similar sight, smell, or phrase pops up, those brain cells fire again.
• The more often they fire, the stronger the connection grows – like a well-trodden path through grass.
Over months or years, these “emotional shortcuts” can hijack the present. A casual remark triggers an outsized reaction; yesterday’s hurt suddenly feels brand-new.
The pain-body in action
When an old wound re-awakens:
1. Body first: Heart races, muscles tense, breath shortens.
2. Mind next: Thoughts narrow, old stories replay (“They always ignore me”).
3. Impulse takes over: We snap, withdraw, or over-explain before we realize what’s happening.
That’s because the brain’s alarm centre (amygdala) has drowned out the wise planner in the front (prefrontal cortex). We’re temporarily running on emotion, not reason.
Breaking the loop
Scientists call the way back “top-down modulation.” In plain English: use the thoughtful part of the brain to calm the reactive part.
• Notice the signal. The moment you feel the surge – name it (“Tight chest… old anger”).
• Shift to sensation. Focus on raw data: the warmth in your face, the thump of your heart. This keeps attention in the present, where the pain-body can’t feed on past stories.
• Breathe and wait. Even 90 seconds of steady breathing lets the chemical storm subside.
• Choose a response. Once calm, the prefrontal cortex switches back on, offering options besides fight, flight, or freeze.
Every time you do this, you weaken the old pathway. Skip the rumination; let the feeling rise and fall without rehearsing the narrative. Starve the pain-body, and it gradually shrinks.
What freedom looks like
The goal isn’t to erase pain – life
will still pinch. Instead, it’s to feel without becoming fused with the feeling. Over time:
• Reactions grow milder and shorter.
• Compassion – for yourself and others – shows up first, not last.
• Choices expand: a pause, a question, a gentle “Let’s talk later.”
Old echoes fade when they’re no longer amplified by our attention. In the new quiet, we can steer by what matters now, not by what once went wrong.
When the past calls, let it go to voicemail. The present moment has better things to say.
GNLM
Photo - Neuroscience News
Emotional suffering is not merely a fleeting mood or psychological abstraction – it is deeply rooted in our neurobiology. The human brain carries the imprint of past pain within its very circuits, shaping how we perceive the world, regulate emotions, and relate to others.
Eckhart Tolle’s concept of the “pain-body” – a reservoir of accumulated emotional pain – finds striking parallels in neuroscience. In particular, the brain’s limbic system, including the amygdala and hippocampus, encodes emotionally charged experiences. These memories are tagged as significant and can be reactivated by seemingly minor cues, often without conscious awareness. Far from fading over time, these emotional imprints are reinforced through repetition, forming feedback loops that keep old wounds alive in the present.
The pain-body, then, can be understood as a neuro-affective pattern, a system of heightened reactivity that feeds on attention, identification, and the constant replaying of personal narratives. When it is activated, we often feel hijacked: our bodies tense, our minds narrow, and we may behave in ways that feel impulsive or out of character. This happens because the prefrontal cortex, the part of the brain responsible for thoughtful decision-making, becomes inhibited, allowing the emotional brain to take control.
The key to dissolving the pain-body lies in disrupting these loops. Neuroscience points to the role of the anterior cingulate cortex, which governs attention. By cultivating present-moment awareness, we engage in what’s known as “top-down modulation” – the intentional use of higher brain functions to regulate emotional responses. This is not passive mindfulness, but active engagement: paying close attention to the raw sensation of emotion, rather than being swept away by the story we tell about it.
The pain-body is nourished by rumination, projection, and emotional fusion. Feeding it strengthens the brain’s synaptic pathways, making emotional reactivity a default state. Over time, suffering becomes a form of identity. To reverse this, we must learn to be still, not as a form of escape, but as a recalibration of the nervous system. Stillness allows us to step out of the cycle, to feel without becoming fused with what is felt.
True transformation doesn’t come from suppression or struggle. It comes from witnessing. In this act of gentle observation, we cease to feed the pain-body. Without attention, it begins to lose its grip. Compassion and presence become the dominant neural patterns. What emerges is not a life without pain, but a self no longer defined by it.
Let the pain-body starve. Let it shrink without your attention. As its voice fades, may you find a quieter mind, a clearer heart, and a presence grounded not in past suffering, but in the freedom to choose anew.
Why Old Hurts Still Echo – and How to Quiet Them
Painful memories aren’t just “in your head”. They live in your brain’s wiring, waiting for the right moment to flare up. This idea, popularized by writer Eckhart Tolle as the “pain-body,” lines up neatly with what neuroscientists see under the microscope.
How pain gets stored
• The limbic system – especially two almond-sized hubs called the amygdala and hippocampus – tags emotional events as important.
• Each time a similar sight, smell, or phrase pops up, those brain cells fire again.
• The more often they fire, the stronger the connection grows – like a well-trodden path through grass.
Over months or years, these “emotional shortcuts” can hijack the present. A casual remark triggers an outsized reaction; yesterday’s hurt suddenly feels brand-new.
The pain-body in action
When an old wound re-awakens:
1. Body first: Heart races, muscles tense, breath shortens.
2. Mind next: Thoughts narrow, old stories replay (“They always ignore me”).
3. Impulse takes over: We snap, withdraw, or over-explain before we realize what’s happening.
That’s because the brain’s alarm centre (amygdala) has drowned out the wise planner in the front (prefrontal cortex). We’re temporarily running on emotion, not reason.
Breaking the loop
Scientists call the way back “top-down modulation.” In plain English: use the thoughtful part of the brain to calm the reactive part.
• Notice the signal. The moment you feel the surge – name it (“Tight chest… old anger”).
• Shift to sensation. Focus on raw data: the warmth in your face, the thump of your heart. This keeps attention in the present, where the pain-body can’t feed on past stories.
• Breathe and wait. Even 90 seconds of steady breathing lets the chemical storm subside.
• Choose a response. Once calm, the prefrontal cortex switches back on, offering options besides fight, flight, or freeze.
Every time you do this, you weaken the old pathway. Skip the rumination; let the feeling rise and fall without rehearsing the narrative. Starve the pain-body, and it gradually shrinks.
What freedom looks like
The goal isn’t to erase pain – life
will still pinch. Instead, it’s to feel without becoming fused with the feeling. Over time:
• Reactions grow milder and shorter.
• Compassion – for yourself and others – shows up first, not last.
• Choices expand: a pause, a question, a gentle “Let’s talk later.”
Old echoes fade when they’re no longer amplified by our attention. In the new quiet, we can steer by what matters now, not by what once went wrong.
When the past calls, let it go to voicemail. The present moment has better things to say.
GNLM
Photo - Neuroscience News

According to one of the objectives of the Social Affairs of State Administration Council (SAC), “To elevate the Health and Sports sectors inclusive of all the people, improving the longevity and health of the nation”, the Ministry of Health (MOH), Myanmar, laid down the two objectives, to enable every citizen to attain total life expectancy and enjoy longevity of life, and to ensure that every citizen is free from diseases. To do that, the newly appointed medical doctors and dentists are the main implementing human resources.
According to one of the objectives of the Social Affairs of State Administration Council (SAC), “To elevate the Health and Sports sectors inclusive of all the people, improving the longevity and health of the nation”, the Ministry of Health (MOH), Myanmar, laid down the two objectives, to enable every citizen to attain total life expectancy and enjoy longevity of life, and to ensure that every citizen is free from diseases. To do that, the newly appointed medical doctors and dentists are the main implementing human resources.
The Chairman of the State Administration Council, Prime Minister Senior General Min Aung Hlaing, attended the ceremony of appointment of new medical doctors and dentists as Government Gazetted Officers on 18 July 2025 at Myanmar Convention Centre, Yangon. At the ceremony, the SAC Chairman delivered a speech that SAC is prioritizing the objective that “nothing is more important than human life” and is striving to provide accessible and high-quality healthcare services to everyone.
He stressed that public hospitals have been organized to provide full-time emergency patient care, and efforts are being made to minimize out-of-pocket expenses for patients by reducing the costs through effective planning and resource allocation. He noted that in order to improve the overall health standards of the public and to increase life expectancy, it is essential to strengthen the delivery of primary healthcare services. To achieve this, it is important to adequately produce sufficient human resources in the health sector and assign them responsibilities accordingly.
The Chairman of the SAC continued that the State is continuously supporting the improvement of healthcare standards for ethnic nationalities, with the understanding that only with good health can people work and pursue education. He expressed his pleasure for fresher medical doctors and dentists to serve their duties to provide healthcare services to the people, as health personnel are responsible for resolving health problems of the people as much as possible. In implementing public healthcare services, the Senior General unveiled that the State is implementing effective policies and plans based on the country’s resources in order to take preventive measures to stop the outbreak of diseases, as well as provide high-quality medical treatment in case illnesses occur.


The Chairman of the SAC disclosed that the government is placing great emphasis on ensuring that the public can receive medical treatment in a peaceful and comfortable environment. To that end, it is upgrading and renovating public hospitals, constructing new ones, enhancing disease detection and advanced medical care, and consistently supplying medicines and modern medical equipment.
He urged them that emphasis should be placed on actions such as improving nutrition and living conditions, administering preventive vaccinations, analyzing and addressing mortality rates, and implementing relevant measures effectively in the respective regions where responsibilities are assigned. The Chairman of the SAC presented certificates of State gazetted officer appointment to representatives from four medical universities, while the Joint Secretary gave certificates of State gazetted officer appointment to representatives from two medical universities and the University of Dental Medicine.
In the second session of the ceremony, Union Minister for Health Dr Thet Khaing Win said that the medics should follow the professional ethic, medical ethic, and civil rules and ethics. The Union Minister stated the need to be mature and stable, to view everything with a wide perspective, and to have a sense of responsibility and accountability for being government employees, and to apply their skills for the people and show loyalty to the country and people. Myanmar Medical Council President Dr Myo Khin and Myanmar Dental Council President Dr Paing Soe briefed the ethics to be followed by the medical doctors and dentists. The officials presented order letters to be assigned as assignment of Government Gazetted Officers to the 1,259 new medical doctors from different Universities of Medicine and 21 new dentists at the event.
In addition, congratulations to the newly appointed medical doctors and dentists, and your role is pivotal in not only diagnosing and treating but also in providing comfort, guidance, and hope to those in need. Remember, every challenge you face is an opportunity to grow, and every success is a step forward in your journey to make a difference and embrace your responsibilities with confidence and compassion. That’s a significant achievement and testament to years of hard work and dedication. We hope that all of you can bring success and fulfilment to this noble profession.
Reference
The Global New Light of Myanmar Newspaper dated 19 July 2025
According to one of the objectives of the Social Affairs of State Administration Council (SAC), “To elevate the Health and Sports sectors inclusive of all the people, improving the longevity and health of the nation”, the Ministry of Health (MOH), Myanmar, laid down the two objectives, to enable every citizen to attain total life expectancy and enjoy longevity of life, and to ensure that every citizen is free from diseases. To do that, the newly appointed medical doctors and dentists are the main implementing human resources.
The Chairman of the State Administration Council, Prime Minister Senior General Min Aung Hlaing, attended the ceremony of appointment of new medical doctors and dentists as Government Gazetted Officers on 18 July 2025 at Myanmar Convention Centre, Yangon. At the ceremony, the SAC Chairman delivered a speech that SAC is prioritizing the objective that “nothing is more important than human life” and is striving to provide accessible and high-quality healthcare services to everyone.
He stressed that public hospitals have been organized to provide full-time emergency patient care, and efforts are being made to minimize out-of-pocket expenses for patients by reducing the costs through effective planning and resource allocation. He noted that in order to improve the overall health standards of the public and to increase life expectancy, it is essential to strengthen the delivery of primary healthcare services. To achieve this, it is important to adequately produce sufficient human resources in the health sector and assign them responsibilities accordingly.
The Chairman of the SAC continued that the State is continuously supporting the improvement of healthcare standards for ethnic nationalities, with the understanding that only with good health can people work and pursue education. He expressed his pleasure for fresher medical doctors and dentists to serve their duties to provide healthcare services to the people, as health personnel are responsible for resolving health problems of the people as much as possible. In implementing public healthcare services, the Senior General unveiled that the State is implementing effective policies and plans based on the country’s resources in order to take preventive measures to stop the outbreak of diseases, as well as provide high-quality medical treatment in case illnesses occur.


The Chairman of the SAC disclosed that the government is placing great emphasis on ensuring that the public can receive medical treatment in a peaceful and comfortable environment. To that end, it is upgrading and renovating public hospitals, constructing new ones, enhancing disease detection and advanced medical care, and consistently supplying medicines and modern medical equipment.
He urged them that emphasis should be placed on actions such as improving nutrition and living conditions, administering preventive vaccinations, analyzing and addressing mortality rates, and implementing relevant measures effectively in the respective regions where responsibilities are assigned. The Chairman of the SAC presented certificates of State gazetted officer appointment to representatives from four medical universities, while the Joint Secretary gave certificates of State gazetted officer appointment to representatives from two medical universities and the University of Dental Medicine.
In the second session of the ceremony, Union Minister for Health Dr Thet Khaing Win said that the medics should follow the professional ethic, medical ethic, and civil rules and ethics. The Union Minister stated the need to be mature and stable, to view everything with a wide perspective, and to have a sense of responsibility and accountability for being government employees, and to apply their skills for the people and show loyalty to the country and people. Myanmar Medical Council President Dr Myo Khin and Myanmar Dental Council President Dr Paing Soe briefed the ethics to be followed by the medical doctors and dentists. The officials presented order letters to be assigned as assignment of Government Gazetted Officers to the 1,259 new medical doctors from different Universities of Medicine and 21 new dentists at the event.
In addition, congratulations to the newly appointed medical doctors and dentists, and your role is pivotal in not only diagnosing and treating but also in providing comfort, guidance, and hope to those in need. Remember, every challenge you face is an opportunity to grow, and every success is a step forward in your journey to make a difference and embrace your responsibilities with confidence and compassion. That’s a significant achievement and testament to years of hard work and dedication. We hope that all of you can bring success and fulfilment to this noble profession.
Reference
The Global New Light of Myanmar Newspaper dated 19 July 2025

Public health surveillance is the essential pillar of the healthcare system. It plays a crucial role in protecting communities, guiding public health actions, and improving population health outcomes. Without proper surveillance, health threats can go unnoticed, allowing diseases to spread unchecked and causing significant harm to society.
Public health surveillance is the essential pillar of the healthcare system. It plays a crucial role in protecting communities, guiding public health actions, and improving population health outcomes. Without proper surveillance, health threats can go unnoticed, allowing diseases to spread unchecked and causing significant harm to society.
Public health surveillance is the continuous and systematic collection, orderly consolidation and evaluation of pertinent data with prompt dissemination of results to those who need to know, particularly those who are in a position to take action.
Effective disease control programs rely on effective surveillance and response systems. Strengthening disease surveillance capacity makes countries better identify disease prevention priorities, plan for the best possible health of their populations, sensitize beneficiaries, focus on evidence-based interventions that work and monitor the trends to show impact as well as to detect issues to address.
Public health surveillance provides the scientific and factual database essential to informed decision-making and appropriate public health action. The key objective of surveillance is to provide information to guide interventions.
Public health surveillance is a tool to estimate the health status and behaviour of the populations served by ministries of health, ministries of finance, and donors. Because surveillance can directly measure what is going on in the population, it is useful both for measuring the need for interventions and for directly measuring the effects of interventions. The purpose of surveillance is to empower decision makers to lead and manage more effectively by providing timely, useful evidence.
In the specialized area of surveillance for biologic terrorism, syndromic surveillance refers to active surveillance of syndromes that may be caused by potential agents used by biologic terrorists and sometimes refers to alternative measures such as increases in the use of over-the-counter drugs or increases in calls to emergency departments.
Early Detection and Prevention
One of the most important reasons for public health surveillance is the early detection of disease outbreaks. By continuously monitoring health data, public health officials can quickly identify unusual patterns or increases in illness. For example, if surveillance systems detect a sudden rise in flu cases, they can alert healthcare providers and the public, allowing preventive measures such as vaccination campaigns or public advisories to be put in place. Early detection saves lives, reduces healthcare costs, and limits the spread of disease.
Informed Decision-Making
Accurate and timely data from surveillance systems allows policymakers and healthcare leaders to make informed decisions. Reliable information helps in setting priorities, allocating resources, and designing effective public health interventions. For example, if data shows a high incidence of diabetes in a certain region, targeted education and prevention programmes can be introduced to address lifestyle factors contributing to the problem.
Tracking Long-Term Health Trends
Surveillance is not only important during outbreaks but also for tracking long-term health trends. By analyzing data over years or decades, public health experts can monitor the impact of interventions, identify emerging health threats, and adapt strategies as needed. This long-term monitoring is especially important for chronic diseases, mental health, environmental hazards, and occupational health risks.
Supporting Research and Innovation
Public health surveillance provides valuable data for scientific research. Researchers use surveillance data to study the causes of diseases, evaluate treatment effectiveness, and develop new prevention strategies. Innovations in healthcare, such as new vaccines or public health policies, often rely on information gathered through careful monitoring.
Building Public Trust and Transparency
Transparent reporting of health information builds public trust. When communities are informed about health risks and the measures being taken to protect them, they are more likely to cooperate with public health recommendations. Trust is especially important during public health emergencies, such as pandemics, where community participation is critical for controlling the spread of disease.
In addition, public health surveillance and monitoring are vital for safeguarding the health of populations. They enable early detection of diseases, support informed decision-making, track health trends, contribute to research, and build public trust. Investing in strong surveillance systems is a wise and necessary step for every nation seeking to improve the well-being of its people and prepare for future health challenges.
GNLM
Public health surveillance is the essential pillar of the healthcare system. It plays a crucial role in protecting communities, guiding public health actions, and improving population health outcomes. Without proper surveillance, health threats can go unnoticed, allowing diseases to spread unchecked and causing significant harm to society.
Public health surveillance is the continuous and systematic collection, orderly consolidation and evaluation of pertinent data with prompt dissemination of results to those who need to know, particularly those who are in a position to take action.
Effective disease control programs rely on effective surveillance and response systems. Strengthening disease surveillance capacity makes countries better identify disease prevention priorities, plan for the best possible health of their populations, sensitize beneficiaries, focus on evidence-based interventions that work and monitor the trends to show impact as well as to detect issues to address.
Public health surveillance provides the scientific and factual database essential to informed decision-making and appropriate public health action. The key objective of surveillance is to provide information to guide interventions.
Public health surveillance is a tool to estimate the health status and behaviour of the populations served by ministries of health, ministries of finance, and donors. Because surveillance can directly measure what is going on in the population, it is useful both for measuring the need for interventions and for directly measuring the effects of interventions. The purpose of surveillance is to empower decision makers to lead and manage more effectively by providing timely, useful evidence.
In the specialized area of surveillance for biologic terrorism, syndromic surveillance refers to active surveillance of syndromes that may be caused by potential agents used by biologic terrorists and sometimes refers to alternative measures such as increases in the use of over-the-counter drugs or increases in calls to emergency departments.
Early Detection and Prevention
One of the most important reasons for public health surveillance is the early detection of disease outbreaks. By continuously monitoring health data, public health officials can quickly identify unusual patterns or increases in illness. For example, if surveillance systems detect a sudden rise in flu cases, they can alert healthcare providers and the public, allowing preventive measures such as vaccination campaigns or public advisories to be put in place. Early detection saves lives, reduces healthcare costs, and limits the spread of disease.
Informed Decision-Making
Accurate and timely data from surveillance systems allows policymakers and healthcare leaders to make informed decisions. Reliable information helps in setting priorities, allocating resources, and designing effective public health interventions. For example, if data shows a high incidence of diabetes in a certain region, targeted education and prevention programmes can be introduced to address lifestyle factors contributing to the problem.
Tracking Long-Term Health Trends
Surveillance is not only important during outbreaks but also for tracking long-term health trends. By analyzing data over years or decades, public health experts can monitor the impact of interventions, identify emerging health threats, and adapt strategies as needed. This long-term monitoring is especially important for chronic diseases, mental health, environmental hazards, and occupational health risks.
Supporting Research and Innovation
Public health surveillance provides valuable data for scientific research. Researchers use surveillance data to study the causes of diseases, evaluate treatment effectiveness, and develop new prevention strategies. Innovations in healthcare, such as new vaccines or public health policies, often rely on information gathered through careful monitoring.
Building Public Trust and Transparency
Transparent reporting of health information builds public trust. When communities are informed about health risks and the measures being taken to protect them, they are more likely to cooperate with public health recommendations. Trust is especially important during public health emergencies, such as pandemics, where community participation is critical for controlling the spread of disease.
In addition, public health surveillance and monitoring are vital for safeguarding the health of populations. They enable early detection of diseases, support informed decision-making, track health trends, contribute to research, and build public trust. Investing in strong surveillance systems is a wise and necessary step for every nation seeking to improve the well-being of its people and prepare for future health challenges.
GNLM

Evolution of Yoga
Yoga’s history is deeply rooted in ancient India, with origins possibly dating back over 5,000 years to the Indus-Sarasvati civilization. The earliest written records appear in the Vedic texts, around 1500 BCE. Over time, Yoga evolved into a system of physical, mental and spiritual practices, passed down through generations. Patanjali’s Yoga Sutras, around 200 BCE, provided a comprehensive framework, including the Eight Limbs of Yoga, which are still relevant today. The classical form of Yoga, as outlined by Patanjali in the Yoga Sutras, is known as Ashtanga Yoga, also referred to as Raja Yoga or the Eight-Limbed Path. It’s a holistic system encompassing physical, mental and spiritual practices, aiming for self-realization.
These eight limbs of Ashtanga Yoga are:
1. Yama: Ethical guidelines and restraints.
2. Niyama: Self-disciplinary practices.
3. Asana: Physical postures.
4. Pranayama: Breath control techniques.
5. Pratyahara: Withdrawal of senses from the external world.
6. Dharana: Concentration.
7. Dhyana: Meditation.
8. Samadhi: State of absorption or union with the divine.
In contemporary Bharat, several figures have significantly developed the understanding and practice of Yoga from ancient traditions, while also adapting them to modern contexts. Some prominent names include Swami Vivekananda, Sri Aurobindo, B K S Iyengar, Sri Ravi Shankar and so on. Swami Vivekananda is widely regarded as a key architect of the revival of Yoga in the late 19th and early 20th centuries. He brought the philosophy and practices of Yoga to the West, introducing it to a broader audience and emphasizing its practical aspects for spiritual growth and social reform. His speeches and writings, particularly his 1893 address at the World’s Parliament of Religions, were remarkable. He also developed his own interpretations of Yoga, incorporating elements of Vedanta and other Hindu philosophies. He presented four distinct yet interconnected paths of Yogas, towards spiritual realization and self-discovery: Karma Yoga (the path of action), Bhakti Yoga (the path of devotion). Raja Yoga (the path of concentration and discipline) and Jnana Yoga (the path of knowledge). Each yoga has a unique approach to realizing the divine within, and Vivekananda believed that all four are equally valid paths to enlightenment.
Sri Aurobindo’s “Integral Yoga” offered a comprehensive approach to spiritual evolution, encompassing physical, mental and spiritual development. He integrated Yoga with his larger philosophy of human evolution and the development of a higher consciousness.
With time, many thinkers, philosophers and teachers propagated and promoted Yoga across the Globe with their unique styles. Society values its importance in its day-to-day life.
Impact of Yoga on Well-being
Yoga has significantly evolved and become a prominent part of contemporary wellness practices, moving beyond its traditional roots to encompass diverse styles and applications, each offering unique benefits and approaches. Some of the most common types include Hatha Yoga, Vinyasa, Ashtanga Yoga, Mantra Yoga, Kriya Yoga and so on. These styles differ in their focus on physical postures, breathwork, meditation and energy flow. It’s increasingly recognized for its benefits in stress reduction, promoting mental and physical health and fostering a sense of balance and well-being. Modern Yoga is also integrated into various settings, including schools, corporations and healthcare systems, reflecting its growing relevance in addressing the needs of the modern world.
Yoga is important because it offers numerous physical, mental and emotional benefits, improving overall well-being and promoting a healthier lifestyle. It’s a practice that can help individuals manage stress, enhance flexibility and strength and even improve sleep quality.
The numerous benefits of Yoga offer a holistic development of an individual in the following way:
Physiological Benefits:
• Improved Flexibility and Strength:
Yoga poses (asanas) target various muscle groups, enhancing flexibility and building strength.
• Reduced Risk of Injury:
Increased flexibility and body awareness can help prevent injuries, especially in sports and other physical activities.
• Better Posture and Balance:
Yoga can improve posture, balance and coordination, leading to physiological benefits like better body alignment and stability.
• Improved Cardiovascular Health:
Regular Yoga practice can help lower blood pressure and heart rate, potentially reducing the risk of heart disease.
• Pain Management:
Yoga can be effective in managing various types of chronic pain, such as back pain and arthritis.
Psychological and Emotional Gains:
• Stress Reduction:
Yoga’s emphasis on breathing and mindfulness can help calm the mind and reduce stress hormones.
• Improved Sleep:
Yoga can help relax the body and mind, making it easier to fall asleep and stay asleep.
• Enhanced Mental Clarity and Focus:
Yoga can improve concentration and attention, leading to better cognitive function.
• Emotional Regulation:
Yoga can help individuals become more aware of their emotions and develop healthy coping mechanisms.
• Increased Mindfulness and Self-Awareness:
Yoga fosters a sense of being present in the moment, which can lead to greater self-awareness and improved decision-making.
Path to Inner Awakening:
• Connection to Self and Others:
Yoga encourages a deeper understanding of oneself and one’s place in the world, promoting a sense of inter connectedness.
• Cultivation of Inner Peace and Harmony:
Yoga can help individuals find inner peace and cultivate a sense of balance and harmony in their lives.
Therefore, Yoga is a valuable practice that can enhance physical, mental, and emotional well-being. Its benefits extend beyond physical exercise, offering a holistic approach to health and wellness. It helps an individual to grow and nurture from the Gross to the subtle.
Yoga and Myanmar: The Connection
Yoga has a deep connection with Myanmar’s cultural landscape due to the shared. historical ties with India, where Yoga originated. Myanmar, the land of meditation, emphasizes mindfulness, inner peace and self-discipline. Yoga is becoming increasingly popular in Myanmar, with a number of Yoga studios and centres opening in different cities like Yangon, Bago, Nay Pyi Taw, Bagan, Mandalay, Sittway, etc.
Myanmar is my fourth posting from the Indian Council for Cultural Relations (ICCR) & the Ministry of External Affairs to promote Yoga. The previous countries included- Hungary, Bosnia & Herzegovina, Cambodia, and New Zealand. I have noticed that the people of Myanmar have a keen interest in knowing the Classical form of Yoga from the Yoga texts. Like any other country, they have a deep interest in staying healthy and active. More than 200 Yoga enthusiasts have joined my Yoga classes at the SVCC, Embassy of India in Yangon. The beautiful parks and gardens across Yangon, like Mahabandoola Park, People’s Park, and Kandawgyi Lake, offer an interesting and fresh atmosphere for fitness enthusiasts to practise Yoga, Pilates, Zumba and other healthy activities in large groups. The serene atmosphere in pagodas like Sule Pagoda and Shwedagon Pagoda allows the local people of Myanmar to disconnect from the outside world and connect with the Self. These strong techniques help the local people to balance their thoughts and emotions to face the different problems and situations of life.
As Buddhism spread from India to Myanmar, it carried forward techniques of mindfulness and concentration that complement the science of Yoga. In essence, meditation serves as a profound path to cultivate mindfulness, inner awareness and overall well-being. Yoga evolved as a system for self-realization during the Vedic period, while meditation practices gained prominence with the rise of Buddhism. Both Yoga and meditation in Myanmar emphasize cultivating mindfulness and deep inner awareness. In Yoga, mindfulness is developed through postures, breath control, and meditation, fostering a connection between the body and mind. Similarly, meditation practices in Myanmar, such as Vipassana (insight meditation), centre on observing the present moment with clarity and understanding the true nature of reality. Yoga in Myanmar is gaining popularity as Myanmar’s predominantly Buddhist culture provides a unique context for Yoga practice, with opportunities to integrate Yoga with meditation and spiritual practice. The Embassy of India (SVCC) in Yangon has organized several International Yoga Day celebrations across the country, and many health enthusiasts actively participate in these initiatives. This year, we are celebrating the 11th International Day of Yoga 2025 with the theme “Yoga for One Earth, One Health”, which highlights Yoga’s role in promoting physical, mental and environmental well-being, aligning with global calls for sustainability and unity. The Embassy of India is planning different events to celebrate this year’s International Day of Yoga.
Significance of Yoga for the people of Myanmar
Yoga is gaining significance in Myanmar as a tool for physical and mental well-being, offering benefits like stress reduction, improved flexibility and a deeper connection to the body and mind. It is a way to promote health, prevent disease and cultivate inner peace, aligning with Myanmar’s Buddhist traditions and emphasis on mindfulness. The following are the key benefits which individuals are experiencing in different dimensions:
• Physical Dimension:
Yoga practices can improve physical health by increasing flexibility, strength, and balance. They can also help with managing stress, which is a major factor in many lifestyle-related disorders.
• Mental Dimension:
Yoga’s emphasis on mindfulness and meditation can help reduce stress, anxiety, and depression. It promotes a sense of calm and inner peace, which can be particularly beneficial in a society that values spiritual well-being.
• Spiritual Dimension:
Yoga’s roots, in ancient Indian traditions, including its focus on self-discipline and inner awareness, connect well with Myanmar’s Buddhist culture and its emphasis on meditation and mindfulness. Yoga can deepen understanding of the nature of life and cultivate inner peace, which is valued in Myanmar’s spiritual traditions.
• Social and Cultural Significance:
Yoga is increasingly being recognized as a practice that can promote harmony and well-being in all aspects of life. It’s also becoming a more accessible practice, with yoga studios and instructors becoming more common in Myanmar.
International Recognition:
The celebration of the International Day of Yoga in Myanmar highlights its growing significance and the global recognition of its benefits.
Yoga is therefore gaining popularity in Myanmar and is viewed as a way to promote physical, mental and spiritual well-being. It is often practised in conjunction with meditation, reflecting the influence of Buddhism in the country. Yoga studios and retreats are becoming more common, offering a variety of classes and workshops for different levels of practitioners.
My personal experience in Myanmar so far is a blend of ancient history, vibrant culture, and natural beauty, but the best part about Myanmar is its beautiful people. The love and warmth which I receive from my Yoga students is overwhelming.
GNLM
Evolution of Yoga
Yoga’s history is deeply rooted in ancient India, with origins possibly dating back over 5,000 years to the Indus-Sarasvati civilization. The earliest written records appear in the Vedic texts, around 1500 BCE. Over time, Yoga evolved into a system of physical, mental and spiritual practices, passed down through generations. Patanjali’s Yoga Sutras, around 200 BCE, provided a comprehensive framework, including the Eight Limbs of Yoga, which are still relevant today. The classical form of Yoga, as outlined by Patanjali in the Yoga Sutras, is known as Ashtanga Yoga, also referred to as Raja Yoga or the Eight-Limbed Path. It’s a holistic system encompassing physical, mental and spiritual practices, aiming for self-realization.
These eight limbs of Ashtanga Yoga are:
1. Yama: Ethical guidelines and restraints.
2. Niyama: Self-disciplinary practices.
3. Asana: Physical postures.
4. Pranayama: Breath control techniques.
5. Pratyahara: Withdrawal of senses from the external world.
6. Dharana: Concentration.
7. Dhyana: Meditation.
8. Samadhi: State of absorption or union with the divine.
In contemporary Bharat, several figures have significantly developed the understanding and practice of Yoga from ancient traditions, while also adapting them to modern contexts. Some prominent names include Swami Vivekananda, Sri Aurobindo, B K S Iyengar, Sri Ravi Shankar and so on. Swami Vivekananda is widely regarded as a key architect of the revival of Yoga in the late 19th and early 20th centuries. He brought the philosophy and practices of Yoga to the West, introducing it to a broader audience and emphasizing its practical aspects for spiritual growth and social reform. His speeches and writings, particularly his 1893 address at the World’s Parliament of Religions, were remarkable. He also developed his own interpretations of Yoga, incorporating elements of Vedanta and other Hindu philosophies. He presented four distinct yet interconnected paths of Yogas, towards spiritual realization and self-discovery: Karma Yoga (the path of action), Bhakti Yoga (the path of devotion). Raja Yoga (the path of concentration and discipline) and Jnana Yoga (the path of knowledge). Each yoga has a unique approach to realizing the divine within, and Vivekananda believed that all four are equally valid paths to enlightenment.
Sri Aurobindo’s “Integral Yoga” offered a comprehensive approach to spiritual evolution, encompassing physical, mental and spiritual development. He integrated Yoga with his larger philosophy of human evolution and the development of a higher consciousness.
With time, many thinkers, philosophers and teachers propagated and promoted Yoga across the Globe with their unique styles. Society values its importance in its day-to-day life.
Impact of Yoga on Well-being
Yoga has significantly evolved and become a prominent part of contemporary wellness practices, moving beyond its traditional roots to encompass diverse styles and applications, each offering unique benefits and approaches. Some of the most common types include Hatha Yoga, Vinyasa, Ashtanga Yoga, Mantra Yoga, Kriya Yoga and so on. These styles differ in their focus on physical postures, breathwork, meditation and energy flow. It’s increasingly recognized for its benefits in stress reduction, promoting mental and physical health and fostering a sense of balance and well-being. Modern Yoga is also integrated into various settings, including schools, corporations and healthcare systems, reflecting its growing relevance in addressing the needs of the modern world.
Yoga is important because it offers numerous physical, mental and emotional benefits, improving overall well-being and promoting a healthier lifestyle. It’s a practice that can help individuals manage stress, enhance flexibility and strength and even improve sleep quality.
The numerous benefits of Yoga offer a holistic development of an individual in the following way:
Physiological Benefits:
• Improved Flexibility and Strength:
Yoga poses (asanas) target various muscle groups, enhancing flexibility and building strength.
• Reduced Risk of Injury:
Increased flexibility and body awareness can help prevent injuries, especially in sports and other physical activities.
• Better Posture and Balance:
Yoga can improve posture, balance and coordination, leading to physiological benefits like better body alignment and stability.
• Improved Cardiovascular Health:
Regular Yoga practice can help lower blood pressure and heart rate, potentially reducing the risk of heart disease.
• Pain Management:
Yoga can be effective in managing various types of chronic pain, such as back pain and arthritis.
Psychological and Emotional Gains:
• Stress Reduction:
Yoga’s emphasis on breathing and mindfulness can help calm the mind and reduce stress hormones.
• Improved Sleep:
Yoga can help relax the body and mind, making it easier to fall asleep and stay asleep.
• Enhanced Mental Clarity and Focus:
Yoga can improve concentration and attention, leading to better cognitive function.
• Emotional Regulation:
Yoga can help individuals become more aware of their emotions and develop healthy coping mechanisms.
• Increased Mindfulness and Self-Awareness:
Yoga fosters a sense of being present in the moment, which can lead to greater self-awareness and improved decision-making.
Path to Inner Awakening:
• Connection to Self and Others:
Yoga encourages a deeper understanding of oneself and one’s place in the world, promoting a sense of inter connectedness.
• Cultivation of Inner Peace and Harmony:
Yoga can help individuals find inner peace and cultivate a sense of balance and harmony in their lives.
Therefore, Yoga is a valuable practice that can enhance physical, mental, and emotional well-being. Its benefits extend beyond physical exercise, offering a holistic approach to health and wellness. It helps an individual to grow and nurture from the Gross to the subtle.
Yoga and Myanmar: The Connection
Yoga has a deep connection with Myanmar’s cultural landscape due to the shared. historical ties with India, where Yoga originated. Myanmar, the land of meditation, emphasizes mindfulness, inner peace and self-discipline. Yoga is becoming increasingly popular in Myanmar, with a number of Yoga studios and centres opening in different cities like Yangon, Bago, Nay Pyi Taw, Bagan, Mandalay, Sittway, etc.
Myanmar is my fourth posting from the Indian Council for Cultural Relations (ICCR) & the Ministry of External Affairs to promote Yoga. The previous countries included- Hungary, Bosnia & Herzegovina, Cambodia, and New Zealand. I have noticed that the people of Myanmar have a keen interest in knowing the Classical form of Yoga from the Yoga texts. Like any other country, they have a deep interest in staying healthy and active. More than 200 Yoga enthusiasts have joined my Yoga classes at the SVCC, Embassy of India in Yangon. The beautiful parks and gardens across Yangon, like Mahabandoola Park, People’s Park, and Kandawgyi Lake, offer an interesting and fresh atmosphere for fitness enthusiasts to practise Yoga, Pilates, Zumba and other healthy activities in large groups. The serene atmosphere in pagodas like Sule Pagoda and Shwedagon Pagoda allows the local people of Myanmar to disconnect from the outside world and connect with the Self. These strong techniques help the local people to balance their thoughts and emotions to face the different problems and situations of life.
As Buddhism spread from India to Myanmar, it carried forward techniques of mindfulness and concentration that complement the science of Yoga. In essence, meditation serves as a profound path to cultivate mindfulness, inner awareness and overall well-being. Yoga evolved as a system for self-realization during the Vedic period, while meditation practices gained prominence with the rise of Buddhism. Both Yoga and meditation in Myanmar emphasize cultivating mindfulness and deep inner awareness. In Yoga, mindfulness is developed through postures, breath control, and meditation, fostering a connection between the body and mind. Similarly, meditation practices in Myanmar, such as Vipassana (insight meditation), centre on observing the present moment with clarity and understanding the true nature of reality. Yoga in Myanmar is gaining popularity as Myanmar’s predominantly Buddhist culture provides a unique context for Yoga practice, with opportunities to integrate Yoga with meditation and spiritual practice. The Embassy of India (SVCC) in Yangon has organized several International Yoga Day celebrations across the country, and many health enthusiasts actively participate in these initiatives. This year, we are celebrating the 11th International Day of Yoga 2025 with the theme “Yoga for One Earth, One Health”, which highlights Yoga’s role in promoting physical, mental and environmental well-being, aligning with global calls for sustainability and unity. The Embassy of India is planning different events to celebrate this year’s International Day of Yoga.
Significance of Yoga for the people of Myanmar
Yoga is gaining significance in Myanmar as a tool for physical and mental well-being, offering benefits like stress reduction, improved flexibility and a deeper connection to the body and mind. It is a way to promote health, prevent disease and cultivate inner peace, aligning with Myanmar’s Buddhist traditions and emphasis on mindfulness. The following are the key benefits which individuals are experiencing in different dimensions:
• Physical Dimension:
Yoga practices can improve physical health by increasing flexibility, strength, and balance. They can also help with managing stress, which is a major factor in many lifestyle-related disorders.
• Mental Dimension:
Yoga’s emphasis on mindfulness and meditation can help reduce stress, anxiety, and depression. It promotes a sense of calm and inner peace, which can be particularly beneficial in a society that values spiritual well-being.
• Spiritual Dimension:
Yoga’s roots, in ancient Indian traditions, including its focus on self-discipline and inner awareness, connect well with Myanmar’s Buddhist culture and its emphasis on meditation and mindfulness. Yoga can deepen understanding of the nature of life and cultivate inner peace, which is valued in Myanmar’s spiritual traditions.
• Social and Cultural Significance:
Yoga is increasingly being recognized as a practice that can promote harmony and well-being in all aspects of life. It’s also becoming a more accessible practice, with yoga studios and instructors becoming more common in Myanmar.
International Recognition:
The celebration of the International Day of Yoga in Myanmar highlights its growing significance and the global recognition of its benefits.
Yoga is therefore gaining popularity in Myanmar and is viewed as a way to promote physical, mental and spiritual well-being. It is often practised in conjunction with meditation, reflecting the influence of Buddhism in the country. Yoga studios and retreats are becoming more common, offering a variety of classes and workshops for different levels of practitioners.
My personal experience in Myanmar so far is a blend of ancient history, vibrant culture, and natural beauty, but the best part about Myanmar is its beautiful people. The love and warmth which I receive from my Yoga students is overwhelming.
GNLM

On 20 March 2025, Penn Orthopaedics at the University of Pennsylvania in the United States hosted the annual San Baw, MD, GM ‘58 Honorary Lecture in Orthopaedic Innovation featuring Dr Arnold-Peter C Weiss from the Medical University of South Carolina (MUSC), who was the honorary speaker.
A brief bio-data of Dr San Baw and the youngest person (at the age of 13) to be inserted with an ivory hip prosthesis: Daw Than Htay
On 20 March 2025, Penn Orthopaedics at the University of Pennsylvania in the United States hosted the annual San Baw, MD, GM ‘58 Honorary Lecture in Orthopaedic Innovation featuring Dr Arnold-Peter C Weiss from the Medical University of South Carolina (MUSC), who was the honorary speaker.
A brief bio-data of Dr San Baw and the youngest person (at the age of 13) to be inserted with an ivory hip prosthesis: Daw Than Htay
Dr San Baw (29 June1922-7 December 1984) was my late father.
In January 1960, my late father first used an ivory prosthesis to replace the fractured thigh bone of an 83-year-old Burmese Buddhist nun, Daw Punya. He had to go to an ivory carver in the city of Mandalay to sculpt an ivory hip prosthesis. After his return from the University of Pennsylvania, doing his post-graduate studies for 3 1/2 years, my father was posted as Head of the Department of Orthopaedic Surgery at Mandalay General Hospital from November 1958 to June 1975. And he was posted as chief of orthopaedic surgery at Rangoon (now Yangon) General Hospital from June 1975 until his retirement in October 1980. From 1960 to 1980, Dr San Baw and his junior colleagues operated upon and inserted ivory hip prostheses to replace the fractured thigh bones of patients whose ages ranged from 13 to 87. Definitely one, if not two, persons who Dr San Baw inserted ivory hip prostheses are still alive as of mid-April 2025. On or about December 1969, a person from a village near Mandalay at the age of about thirteen was inserted with an ivory hip prostheses by my late father and his junior colleagues in an operation which lasted for about four hours (as told to me by the patient herself). The patient’s name is Daw Than Htay (born around November 1956). Up till about mid-2021, she lived in a village about a hundred and fifty miles from Mandalay. She currently lives in a monastery in Mandalay. Sometime in 2024, an X Ray was taken of her left hip (about 55 years after her insertion of the ivory prosthesis), and even though the prosthesis was broken, there has been a creeping substitution or ‘biological bonding’ between bone and ivory, the 2024 X-rays show.
Abstract of Presentation at British Orthopaedic Conference in 1969 and Master of Medical Science thesis at the University of Pennsylvania in 1957
My late father was invited by the British Orthopaedic Association to deliver his research on ivory hip prostheses at the annual conference of the British Orthopaedic Association (BOA) in London, which was held from September 23 to 27, 1969. But only an abstract of my father’s presentation was published in the Journal of Bone and Joint Surgery (British volume), Volume 59 B. When I wrote to the BOA sometime around 2019, they stated that they do not have the full paper any more with them. It is ironic that a paper that was presented to the BOA in 1969 is not on record with the BOA but a Master of Medical Science (Orthopaedics) thesis presented to the Department of Orthopaedic Surgery at the then Graduate School of Medicine of the University of Pennsylvania by my late father in late 1957 is in the repository of the University of Pennsylvania library.
No killing of elephants in Burma when ivory prostheses were being used for the non-reunion of the femoral head
In the context of Burma from the 1960s to the early 1990s, ivory was a cheaper material to use as implants or prostheses to replace fractured thigh bones. Starting from 1959 in Mandalay, Dr San Baw studied the physical, mechanical, chemical and biological properties of ivory for about a year before he inserted it as a replacement on the 83-year-old Burmese Buddhist nun Daw Punya in January 1960. He consulted a physics professor and a zoology professor when investigating the physical, mechanical and biological properties of ivory. It must be emphasized that when my father was using ivory to replace hip fractures from the 1960s to early 1980s, there was no (no) killing of elephants. Only when elephants died say carrying logs after living their natural lives, was the ivory extracted from the elephants. Indeed, about ten years after Dr San Baw passed away in December 1984, his junior colleagues continued to use ivory prostheses as hip implants. One such patient, now deceased, Daw (Mrs, honorific) Than Than (May 1923-May 2023) (a different person from Daw Than Htay mentioned above) had a fall and fractured her left hip sometime after 1990. Professor U Meik, a junior colleague of Dr San Baw, an orthopaedic surgeon in Mandalay, used an ivory hip prosthesis in the early 1990s as a hip replacement for Daw Than Than. In October 2014, the elderly lady broke her right hip, and another orthopaedic surgeon replaced it with a metal hip prosthesis
Cover Story in Clinical Orthopaedics Journal of Dr San Baw’s work and Inaugural San Baw Lecture in Orthopaedic Innovation
In August 2017, Clinical Orthopaedics Journal published the case of the only person in the world then over the age of ninety years who had an ivory prosthesis in her left hip and metal prostheses in her right hip, with photos of X-rays. On the cover of the Journal, the photos of ivory hip prostheses that yours truly sent to the Journal were ‘touched up’ and displayed.
In December 2017, I contributed funds to the Department of Orthopaedic Surgery at the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania to establish an annual Lecture in perpetuity in my father’s name: ‘San Baw, MD. GM’58 Honorary Lecture in Orthopaedic Innovation’.
On 29 November 2018, Dr Bartek Szostakowski, a Polish orthopaedic surgeon at the Maria Sklodowska Curie Memorial Cancer Centre and Institute of Oncology in Warsaw, Poland, gave the inaugural ‘San Baw, Honorary Lecture in Orthopaedic Innovation’ titled ‘Dr San Baw, a forgotten innovator in orthopaedic biologic reconstruction’. I also gave a presentation, ‘Dr San Baw: A Son’s Tribute to an Ivory Prince’. From 2022 to 2025, there have been four San Baw Lectures in Orthopaedic innovation that were held at the University of Pennsylvania in honour of Dr San Baw. After the two inaugural Lectures by me and Dr Bartek, Dr L Scott Levin, Chair of Orthopaedic Surgery at Penn, stated that ‘San Baw was an innovative, compassionate physician who pioneered techniques in hip arthroplasty … We are delighted to perpetuate the legacy of this remarkable orthopaedic surgeon’.
Scant domestic and international recognition in relation to Dr San Baw’s contributions
Sir John Charnley (29 August 1911-5 August 1982), a British orthopaedic surgeon, was recognised as the founder of modern hip replacement (total hip arthroplasty) and, in layperson’s terms, one of the leading pioneers of metal hip prostheses. When he passed away in 1982, there was a short obituary of him in the New York Times. (26 August 1982, Section B, page 12). In 1990, British orthopaedic surgeon William Waugh (17 February 1922-21 May 1998) published a biography of Sir John, titled John Charnley [:] The Man and the Hip (Springer-Verlag).
The next year in 1983, another pioneer of vitallium hip prostheses, an American orthopaedic surgeon, Dr Frederick Thompson (1907-April 12,1983), passed away. The New York Times also published a longer obituary on its 15 April 1983 issue (Section D at page 18). But when Dr San Baw passed away just over 1 ½ years after Dr Frederick Thompson and just over 2 years after Sir John Charnley did, forget the New York Times, not even local Burmese and English language newspapers carried the news.
But I should say that about 10 of the newspapers in the United States did carry a news item under various headings, including ‘Ivory replaces metal in bone transplants’ written by journalist Albert E Kaff (1920-October 2011) in January and February 1970 issues. After my father passed away, I saw three handwritten letters addressed to my father, ‘Dr San Baw, Mandalay General Hospital, Mandalay, Burma’. The letters all came from the United States asking my father’s advice for their orthopaedic problems. One of the correspondents attached a cutting of a news item under the above title from the San Bernardino County Sun newspaper of 31 January 1970. Albert E Kaff was reporting on the ‘Lecture Dr San Baw at the British Orthopaedic Association in London in September 1969’, the UPI report by Albert E Kaff might have reached the Editors’ desk of the New York Times in early 1970, they might not have published it.
Ivory prostheses sample and prosthetic work being done ‘in Malaysia’: A correction
Still, smidgens (so to speak) of recognition somewhat belatedly came. There is a display (since when I do not know) of a sample of ivory prosthesis in the Museum of Surgery in Edinburgh, Scotland, Great Britain. I was not aware of the display at the museum until a former student wrote to me in 2017 about it. Ms Teo Ju-li, a Malaysian student, was then studying for her Master of Laws (LLM) at the University of Edinburgh, and she visited the Museum. She saw the ivory prosthesis on display and wrote to me about it. At my request, an official of the Museum sent me a photo of the ivory hip prosthesis on display at the Museum of Surgery. It wrongly and briefly stated that it was from ‘Malaysia’. I sent a few documents concerning my late father, and the museum personnel kindly changed it to QUOTE ‘Burma (1970). Dr San Baw first used an ivory prosthesis on a Burmese Buddhist nun in 1960. Over 300 prostheses were used in 20 years with 90 per cent success, where patients were able to walk, squat and play football.’ UNQUOTE
The ‘mistake’ of Malaysia for Burma/Myanmar is made not only by the Museum of Surgery in Edinburgh. In a 90-second brief introduction of my late father in the 5th San Baw Honorary Lecture in Orthopaedic Innovation on March 20, 2025 (as indicated above), the introducer correctly stated that Dr San Baw worked at MGH (Mandalay General Hospital) and RGH (Rangoon General Hospital). But in the video link provided to me, where the Lecture was recorded, it was stated that these were the two medical hospitals in ‘Malaysia’ (not Burma) or Myanmar. I should say, though, that in the pamphlet distributed before and during the Lecture, the information regarding my father and Burmese background is correctly stated.
A Malaysian patient and Australian colleagues of Dr San Baw
As it was, Dr San Baw has had some Malaysian and Australian connections as well. From January to June 1976, on a World Health Organization (WHO) Fellowship, he visited orthopaedic centres in Malaysia, Singapore, Australia and Hong Kong. He was in Malaysia in January 1976, visiting the Department of Orthopaedic Surgery at the University of Malaya Hospital. The then Head of the Department of Orthopaedic Surgery at the University of Malaya (UM) Hospital, the late Professor Dr Subramaniam, personally told me in 1990 that Dr San Baw treated the then Malaysian kid who had extra shin bone (infantile pseudarthrosis of the tibia) with his own technique. Incidentally even though BOA only published a 311word abstract of my father’s presentation in the Journal of Bone and Joint Surgery (British volume) (JBJS) in 1970 it did publish in full Dr San Baw’s article ‘The Transarticular graft for infantile pseudarthrosis of the tibia: A New Technique’ in Volume 57 (1975) of the above journal. Again, it is ironic that 14 case studies over a period of eight years on infantile pseudarthrosis were published in full in JBJS in 1975, but 100-plus studies on the insertion of ivory prostheses over a period of nine years were published only in abstract form five years earlier in 1970. But as the late Dr Subramaniam told me, a non-Burmese Malaysian boy (as he then was) in 1976 was also the beneficiary of my father’s innovative technique and compassion.
During his 1976 visit, Dr San Baw spent about two to three months in Australia visiting orthopaedic centres in Brisbane, Sydney, Melbourne, Adelaide and Perth. I am in contact with only one Australian orthopaedic surgeon whom my father met in Australia and who, between 1976 and 2018, has visited Burma/Myanmar about 16 times. He is Emeritus Clinical Professor in Orthopaedics, Dr Robert Bauze of the University of Adelaide. It was in Australia, I understand, that Dr San Baw was called ‘ivory prince’.
Expression of thanks to Australian Colleagues, to Dr Bartek and Dr San Baw’s junior colleagues
I am grateful to Professor Bauze for his many visits to Burma/Myanmar and his assistance in facilitating Burmese orthopaedists and other medical doctors to get their training in Australia and for the Australian health aid projects in Myanmar. I am also grateful to Dr Bartek, as stated above, for re-introducing, reviving the ‘forgotten innovator’ Dr San Baw’s contributions to orthopaedics. Also, my thanks to former junior colleagues of Dr San Baw, Dr (Bobby) Sein Lwin (Florida), Professor Dr Kyaw Myint Naing (Yangon) My father Dr San Baw had in a small corner of the world assiduously and devotedly worked for the welfare of several hundred patients and had trained Burmese orthopaedic surgeons with dedication and compassion.
Source: The Global New Light of Myanmar
On 20 March 2025, Penn Orthopaedics at the University of Pennsylvania in the United States hosted the annual San Baw, MD, GM ‘58 Honorary Lecture in Orthopaedic Innovation featuring Dr Arnold-Peter C Weiss from the Medical University of South Carolina (MUSC), who was the honorary speaker.
A brief bio-data of Dr San Baw and the youngest person (at the age of 13) to be inserted with an ivory hip prosthesis: Daw Than Htay
Dr San Baw (29 June1922-7 December 1984) was my late father.
In January 1960, my late father first used an ivory prosthesis to replace the fractured thigh bone of an 83-year-old Burmese Buddhist nun, Daw Punya. He had to go to an ivory carver in the city of Mandalay to sculpt an ivory hip prosthesis. After his return from the University of Pennsylvania, doing his post-graduate studies for 3 1/2 years, my father was posted as Head of the Department of Orthopaedic Surgery at Mandalay General Hospital from November 1958 to June 1975. And he was posted as chief of orthopaedic surgery at Rangoon (now Yangon) General Hospital from June 1975 until his retirement in October 1980. From 1960 to 1980, Dr San Baw and his junior colleagues operated upon and inserted ivory hip prostheses to replace the fractured thigh bones of patients whose ages ranged from 13 to 87. Definitely one, if not two, persons who Dr San Baw inserted ivory hip prostheses are still alive as of mid-April 2025. On or about December 1969, a person from a village near Mandalay at the age of about thirteen was inserted with an ivory hip prostheses by my late father and his junior colleagues in an operation which lasted for about four hours (as told to me by the patient herself). The patient’s name is Daw Than Htay (born around November 1956). Up till about mid-2021, she lived in a village about a hundred and fifty miles from Mandalay. She currently lives in a monastery in Mandalay. Sometime in 2024, an X Ray was taken of her left hip (about 55 years after her insertion of the ivory prosthesis), and even though the prosthesis was broken, there has been a creeping substitution or ‘biological bonding’ between bone and ivory, the 2024 X-rays show.
Abstract of Presentation at British Orthopaedic Conference in 1969 and Master of Medical Science thesis at the University of Pennsylvania in 1957
My late father was invited by the British Orthopaedic Association to deliver his research on ivory hip prostheses at the annual conference of the British Orthopaedic Association (BOA) in London, which was held from September 23 to 27, 1969. But only an abstract of my father’s presentation was published in the Journal of Bone and Joint Surgery (British volume), Volume 59 B. When I wrote to the BOA sometime around 2019, they stated that they do not have the full paper any more with them. It is ironic that a paper that was presented to the BOA in 1969 is not on record with the BOA but a Master of Medical Science (Orthopaedics) thesis presented to the Department of Orthopaedic Surgery at the then Graduate School of Medicine of the University of Pennsylvania by my late father in late 1957 is in the repository of the University of Pennsylvania library.
No killing of elephants in Burma when ivory prostheses were being used for the non-reunion of the femoral head
In the context of Burma from the 1960s to the early 1990s, ivory was a cheaper material to use as implants or prostheses to replace fractured thigh bones. Starting from 1959 in Mandalay, Dr San Baw studied the physical, mechanical, chemical and biological properties of ivory for about a year before he inserted it as a replacement on the 83-year-old Burmese Buddhist nun Daw Punya in January 1960. He consulted a physics professor and a zoology professor when investigating the physical, mechanical and biological properties of ivory. It must be emphasized that when my father was using ivory to replace hip fractures from the 1960s to early 1980s, there was no (no) killing of elephants. Only when elephants died say carrying logs after living their natural lives, was the ivory extracted from the elephants. Indeed, about ten years after Dr San Baw passed away in December 1984, his junior colleagues continued to use ivory prostheses as hip implants. One such patient, now deceased, Daw (Mrs, honorific) Than Than (May 1923-May 2023) (a different person from Daw Than Htay mentioned above) had a fall and fractured her left hip sometime after 1990. Professor U Meik, a junior colleague of Dr San Baw, an orthopaedic surgeon in Mandalay, used an ivory hip prosthesis in the early 1990s as a hip replacement for Daw Than Than. In October 2014, the elderly lady broke her right hip, and another orthopaedic surgeon replaced it with a metal hip prosthesis
Cover Story in Clinical Orthopaedics Journal of Dr San Baw’s work and Inaugural San Baw Lecture in Orthopaedic Innovation
In August 2017, Clinical Orthopaedics Journal published the case of the only person in the world then over the age of ninety years who had an ivory prosthesis in her left hip and metal prostheses in her right hip, with photos of X-rays. On the cover of the Journal, the photos of ivory hip prostheses that yours truly sent to the Journal were ‘touched up’ and displayed.
In December 2017, I contributed funds to the Department of Orthopaedic Surgery at the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania to establish an annual Lecture in perpetuity in my father’s name: ‘San Baw, MD. GM’58 Honorary Lecture in Orthopaedic Innovation’.
On 29 November 2018, Dr Bartek Szostakowski, a Polish orthopaedic surgeon at the Maria Sklodowska Curie Memorial Cancer Centre and Institute of Oncology in Warsaw, Poland, gave the inaugural ‘San Baw, Honorary Lecture in Orthopaedic Innovation’ titled ‘Dr San Baw, a forgotten innovator in orthopaedic biologic reconstruction’. I also gave a presentation, ‘Dr San Baw: A Son’s Tribute to an Ivory Prince’. From 2022 to 2025, there have been four San Baw Lectures in Orthopaedic innovation that were held at the University of Pennsylvania in honour of Dr San Baw. After the two inaugural Lectures by me and Dr Bartek, Dr L Scott Levin, Chair of Orthopaedic Surgery at Penn, stated that ‘San Baw was an innovative, compassionate physician who pioneered techniques in hip arthroplasty … We are delighted to perpetuate the legacy of this remarkable orthopaedic surgeon’.
Scant domestic and international recognition in relation to Dr San Baw’s contributions
Sir John Charnley (29 August 1911-5 August 1982), a British orthopaedic surgeon, was recognised as the founder of modern hip replacement (total hip arthroplasty) and, in layperson’s terms, one of the leading pioneers of metal hip prostheses. When he passed away in 1982, there was a short obituary of him in the New York Times. (26 August 1982, Section B, page 12). In 1990, British orthopaedic surgeon William Waugh (17 February 1922-21 May 1998) published a biography of Sir John, titled John Charnley [:] The Man and the Hip (Springer-Verlag).
The next year in 1983, another pioneer of vitallium hip prostheses, an American orthopaedic surgeon, Dr Frederick Thompson (1907-April 12,1983), passed away. The New York Times also published a longer obituary on its 15 April 1983 issue (Section D at page 18). But when Dr San Baw passed away just over 1 ½ years after Dr Frederick Thompson and just over 2 years after Sir John Charnley did, forget the New York Times, not even local Burmese and English language newspapers carried the news.
But I should say that about 10 of the newspapers in the United States did carry a news item under various headings, including ‘Ivory replaces metal in bone transplants’ written by journalist Albert E Kaff (1920-October 2011) in January and February 1970 issues. After my father passed away, I saw three handwritten letters addressed to my father, ‘Dr San Baw, Mandalay General Hospital, Mandalay, Burma’. The letters all came from the United States asking my father’s advice for their orthopaedic problems. One of the correspondents attached a cutting of a news item under the above title from the San Bernardino County Sun newspaper of 31 January 1970. Albert E Kaff was reporting on the ‘Lecture Dr San Baw at the British Orthopaedic Association in London in September 1969’, the UPI report by Albert E Kaff might have reached the Editors’ desk of the New York Times in early 1970, they might not have published it.
Ivory prostheses sample and prosthetic work being done ‘in Malaysia’: A correction
Still, smidgens (so to speak) of recognition somewhat belatedly came. There is a display (since when I do not know) of a sample of ivory prosthesis in the Museum of Surgery in Edinburgh, Scotland, Great Britain. I was not aware of the display at the museum until a former student wrote to me in 2017 about it. Ms Teo Ju-li, a Malaysian student, was then studying for her Master of Laws (LLM) at the University of Edinburgh, and she visited the Museum. She saw the ivory prosthesis on display and wrote to me about it. At my request, an official of the Museum sent me a photo of the ivory hip prosthesis on display at the Museum of Surgery. It wrongly and briefly stated that it was from ‘Malaysia’. I sent a few documents concerning my late father, and the museum personnel kindly changed it to QUOTE ‘Burma (1970). Dr San Baw first used an ivory prosthesis on a Burmese Buddhist nun in 1960. Over 300 prostheses were used in 20 years with 90 per cent success, where patients were able to walk, squat and play football.’ UNQUOTE
The ‘mistake’ of Malaysia for Burma/Myanmar is made not only by the Museum of Surgery in Edinburgh. In a 90-second brief introduction of my late father in the 5th San Baw Honorary Lecture in Orthopaedic Innovation on March 20, 2025 (as indicated above), the introducer correctly stated that Dr San Baw worked at MGH (Mandalay General Hospital) and RGH (Rangoon General Hospital). But in the video link provided to me, where the Lecture was recorded, it was stated that these were the two medical hospitals in ‘Malaysia’ (not Burma) or Myanmar. I should say, though, that in the pamphlet distributed before and during the Lecture, the information regarding my father and Burmese background is correctly stated.
A Malaysian patient and Australian colleagues of Dr San Baw
As it was, Dr San Baw has had some Malaysian and Australian connections as well. From January to June 1976, on a World Health Organization (WHO) Fellowship, he visited orthopaedic centres in Malaysia, Singapore, Australia and Hong Kong. He was in Malaysia in January 1976, visiting the Department of Orthopaedic Surgery at the University of Malaya Hospital. The then Head of the Department of Orthopaedic Surgery at the University of Malaya (UM) Hospital, the late Professor Dr Subramaniam, personally told me in 1990 that Dr San Baw treated the then Malaysian kid who had extra shin bone (infantile pseudarthrosis of the tibia) with his own technique. Incidentally even though BOA only published a 311word abstract of my father’s presentation in the Journal of Bone and Joint Surgery (British volume) (JBJS) in 1970 it did publish in full Dr San Baw’s article ‘The Transarticular graft for infantile pseudarthrosis of the tibia: A New Technique’ in Volume 57 (1975) of the above journal. Again, it is ironic that 14 case studies over a period of eight years on infantile pseudarthrosis were published in full in JBJS in 1975, but 100-plus studies on the insertion of ivory prostheses over a period of nine years were published only in abstract form five years earlier in 1970. But as the late Dr Subramaniam told me, a non-Burmese Malaysian boy (as he then was) in 1976 was also the beneficiary of my father’s innovative technique and compassion.
During his 1976 visit, Dr San Baw spent about two to three months in Australia visiting orthopaedic centres in Brisbane, Sydney, Melbourne, Adelaide and Perth. I am in contact with only one Australian orthopaedic surgeon whom my father met in Australia and who, between 1976 and 2018, has visited Burma/Myanmar about 16 times. He is Emeritus Clinical Professor in Orthopaedics, Dr Robert Bauze of the University of Adelaide. It was in Australia, I understand, that Dr San Baw was called ‘ivory prince’.
Expression of thanks to Australian Colleagues, to Dr Bartek and Dr San Baw’s junior colleagues
I am grateful to Professor Bauze for his many visits to Burma/Myanmar and his assistance in facilitating Burmese orthopaedists and other medical doctors to get their training in Australia and for the Australian health aid projects in Myanmar. I am also grateful to Dr Bartek, as stated above, for re-introducing, reviving the ‘forgotten innovator’ Dr San Baw’s contributions to orthopaedics. Also, my thanks to former junior colleagues of Dr San Baw, Dr (Bobby) Sein Lwin (Florida), Professor Dr Kyaw Myint Naing (Yangon) My father Dr San Baw had in a small corner of the world assiduously and devotedly worked for the welfare of several hundred patients and had trained Burmese orthopaedic surgeons with dedication and compassion.
Source: The Global New Light of Myanmar
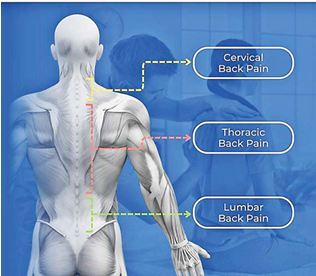
Hitting 10,000 steps a day is a goal for millions of us. But the number of minutes we walk for may be a more important target to focus on.
Scientists believe being on your feet for over an hour-and-a-half every day could slash the risk of chronic lower back pain.
Norwegian and Danish researchers found people who walk for over 100 minutes a day cut this risk by almost a quarter compared to those who clocked 78 minutes per day or less.
Hitting 10,000 steps a day is a goal for millions of us. But the number of minutes we walk for may be a more important target to focus on.
Scientists believe being on your feet for over an hour-and-a-half every day could slash the risk of chronic lower back pain.
Norwegian and Danish researchers found people who walk for over 100 minutes a day cut this risk by almost a quarter compared to those who clocked 78 minutes per day or less.
They also discovered faster walkers were less likely to have chronic back pain—but the effect was less pronounced than walking for longer.
Experts, who labelled the findings important, urged policy makers to push walking as a 'public health strategy' to reduce the risk of the agonising condition.
In many cases, lower back pain starts suddenly and improves within a few days or weeks.
But if it sticks around for more than three months, it’s classed as chronic, according to the NHS. In some cases, it can be considered a disability.
In the study, 11,194 Norwegians, with an average age of 55, were quizzed on their health and how much exercise they did per week.
Almost a sixth (14.8 per cent) reported suffering from lower back pain, answering 'yes' to the following questions, 'During the last year, have you had pain and/or stiffness in your muscles or joints that lasted for at least three consecutive months? and 'Where have you had this pain or stiffness?'
Participants were considered to have the condition if they answered yes to the first question and reported pain in the lower back to the second.
Both men and women were involved in the study, and 100 minutes was found to be the optimum length of time for both sexes, and all ages.
Writing in the journal JAMA Network Open, the researchers concluded: ‘Compared with walking less than 78 minutes per day, those who walked more than 100 minutes per day had a 23 per cent reduced risk of chronic lower back pain.
'The reduction in risk of chronic lower back pain leveled off beyond a walking volume of about 100 minutes per day.
‘Our findings suggest that daily walking volume is more important than mean walking intensity in reducing the risk of chronic lower back pain.
‘These findings suggest that policies and public health strategies promoting walking could help to reduce the occurrence of chronic lower back pain.’
The researchers also noted that their results are ‘likely generalisable beyond the Norwegian adult population, as physical inactivity prevalence in Norway is comparable to that observed in other high-income countries’.
They did note some limitations of the study, including that participants with higher walking volume tended to exercise more often and reported higher physical work demands, which might give them a physical advantage over other members of the group.
In the UK, musculoskeletal conditions (MSK)—including back pain—are the second biggest reason for people being ‘economically inactive’—where someone is out of work and not looking for work.
Figures released by the Government in December 2024 revealed that MSK conditions affect approximately 646,000 Britons, 1-in-4 of the 2.8m who are claiming long-term sickness benefits.
MSK comes second only to mental health issues for reasons why people are unable to work.
It was estimated that 23.4 million working days in the UK were lost due to MSK conditions in 2022.
NHS waiting lists for MSK community services are the highest of all community waits in England, with 348,799 people in September 2024 waiting to see a specialist.
As part of their Get Britain Working White Paper, the Government pledged a £3.5million package to 17 Integrated Care Boards (ICBs) across England to improve local MSK services.
Mail Online
Hitting 10,000 steps a day is a goal for millions of us. But the number of minutes we walk for may be a more important target to focus on.
Scientists believe being on your feet for over an hour-and-a-half every day could slash the risk of chronic lower back pain.
Norwegian and Danish researchers found people who walk for over 100 minutes a day cut this risk by almost a quarter compared to those who clocked 78 minutes per day or less.
They also discovered faster walkers were less likely to have chronic back pain—but the effect was less pronounced than walking for longer.
Experts, who labelled the findings important, urged policy makers to push walking as a 'public health strategy' to reduce the risk of the agonising condition.
In many cases, lower back pain starts suddenly and improves within a few days or weeks.
But if it sticks around for more than three months, it’s classed as chronic, according to the NHS. In some cases, it can be considered a disability.
In the study, 11,194 Norwegians, with an average age of 55, were quizzed on their health and how much exercise they did per week.
Almost a sixth (14.8 per cent) reported suffering from lower back pain, answering 'yes' to the following questions, 'During the last year, have you had pain and/or stiffness in your muscles or joints that lasted for at least three consecutive months? and 'Where have you had this pain or stiffness?'
Participants were considered to have the condition if they answered yes to the first question and reported pain in the lower back to the second.
Both men and women were involved in the study, and 100 minutes was found to be the optimum length of time for both sexes, and all ages.
Writing in the journal JAMA Network Open, the researchers concluded: ‘Compared with walking less than 78 minutes per day, those who walked more than 100 minutes per day had a 23 per cent reduced risk of chronic lower back pain.
'The reduction in risk of chronic lower back pain leveled off beyond a walking volume of about 100 minutes per day.
‘Our findings suggest that daily walking volume is more important than mean walking intensity in reducing the risk of chronic lower back pain.
‘These findings suggest that policies and public health strategies promoting walking could help to reduce the occurrence of chronic lower back pain.’
The researchers also noted that their results are ‘likely generalisable beyond the Norwegian adult population, as physical inactivity prevalence in Norway is comparable to that observed in other high-income countries’.
They did note some limitations of the study, including that participants with higher walking volume tended to exercise more often and reported higher physical work demands, which might give them a physical advantage over other members of the group.
In the UK, musculoskeletal conditions (MSK)—including back pain—are the second biggest reason for people being ‘economically inactive’—where someone is out of work and not looking for work.
Figures released by the Government in December 2024 revealed that MSK conditions affect approximately 646,000 Britons, 1-in-4 of the 2.8m who are claiming long-term sickness benefits.
MSK comes second only to mental health issues for reasons why people are unable to work.
It was estimated that 23.4 million working days in the UK were lost due to MSK conditions in 2022.
NHS waiting lists for MSK community services are the highest of all community waits in England, with 348,799 people in September 2024 waiting to see a specialist.
As part of their Get Britain Working White Paper, the Government pledged a £3.5million package to 17 Integrated Care Boards (ICBs) across England to improve local MSK services.
Mail Online

Why is cycling one of the best Exercises for every lifestyle? In a world where people are becoming more aware of the importance of maintaining physical and mental health, finding the right form of exercise is key. For many, the solution might be simpler – and more enjoyable – than they think: cycling.
Why is cycling one of the best Exercises for every lifestyle? In a world where people are becoming more aware of the importance of maintaining physical and mental health, finding the right form of exercise is key. For many, the solution might be simpler – and more enjoyable – than they think: cycling.
Whether you’re cruising down a quiet neighbourhood road, commuting to work, joining a spin class at the gym, or pedalling at home on a stationary bike, cycling is a powerful and flexible form of exercise. Not only does it improve physical health, but it also supports mental well-being, offers practical lifestyle benefits, and even helps protect the environment.
Let’s explore why cycling continues to gain popularity around the world and why it might just be the perfect activity to incorporate into your life – no matter your age, schedule, or fitness level.
An Exercise That Moves Your Heart (Literally)
One of the most celebrated benefits of cycling is how it supports heart health. As an aerobic exercise, cycling increases your heart rate and improves blood circulation throughout your body. Studies have shown that regular cyclists tend to have lower blood pressure and resting heart rates compared to inactive people.
Research has also revealed that people who cycle regularly are at a significantly reduced risk of developing coronary heart disease or suffering a heart attack. That’s because cycling helps keep your heart strong and arteries clear, reducing strain on the cardiovascular system. Just a few sessions a week, even at a moderate pace, can dramatically improve your cardiovascular fitness.
Gentle on the Joints, Powerful in Impact
Unlike activities such as running, which place repeated stress on your joints, cycling is a low-impact activity. This makes it especially appealing for people with joint issues, older adults, or those recovering from injuries.
Cycling is commonly used in physical therapy and rehabilitation programs. It promotes mobility, increases range of motion, and improves strength – all without putting your knees, hips, and ankles under heavy pressure.
A 2024 study found that people with osteoarthritis who incorporated cycling into their weekly routine experienced less knee pain than non-cyclists. This shows how effective and gentle cycling can be for long-term joint health.
Maintaining a Healthy Weight Made Easier
Weight management is a challenge for many, especially with busy schedules and sedentary lifestyles. Fortunately, cycling provides a fun, convenient way to help keep your weight in check. Regular cyclists often maintain a healthier body composition, which refers to the balance between fat, muscle, bone, and water in the body. Cycling burns calories, builds muscle, and boosts metabolism – all of which are essential for weight control.
The Centres for Disease Control and Prevention (CDC) recommends at least 150 minutes of moderate-intensity aerobic activity each week. Cycling is a great way to meet that recommendation. Whether you bike for 30 minutes five days a week or do three 50-minute sessions, you’ll be helping your body stay fit and active.
Want to lose weight? Increase your intensity by riding uphill, speeding up your pace, or extending your cycling sessions. These adjustments will boost your calorie burn and help you reach your goals faster.
Boost Your Mood, Beat the Blues
Exercise doesn’t just make your body stronger – it lifts your spirits, too. Physical activities like cycling release endorphins, the “feel-good” chemicals that improve mood and reduce stress.
People who cycle regularly often report better sleep, lower levels of anxiety and depression, and an overall improved sense of well-being. Whether it’s the rhythmic motion of pedalling or the calming effect of fresh air and sunshine, biking can be a great mental escape.
Cycling outdoors adds another layer of benefits. Being in nature, enjoying the scenery, and soaking in sunlight can help fight seasonal mood disorders and brighten your day, even after just a short ride.
Preventing Type 2 Diabetes Through Pedal Power
Cycling can play a key role in preventing chronic diseases such as type 2 diabetes. This condition is often linked to poor lifestyle habits, including a lack of physical activity and unhealthy weight gain. By promoting weight control and improving insulin sensitivity, cycling helps your body better regulate blood sugar levels. Studies have shown that people who bike to work or use cycling as a form of exercise have a significantly lower risk of developing type 2 diabetes.
Making cycling a part of your daily or weekly routine could be one of the simplest ways to protect your long-term health.
More Than Exercise: A Lifestyle Choice with Real-World Benefits
Cycling isn’t just a workout – it’s also a practical and sustainable way to live. When used as a mode of transportation, biking helps you save money on gas, parking, and public transport. It also reduces wear and tear on your vehicle and minimizes your carbon footprint. Each time you choose a bike over a car, you’re reducing greenhouse gas emissions. This is a powerful way to combat climate change and improve air quality in your community. Cleaner air leads to better public health and fewer respiratory issues, especially for children and the elderly.
Cycling can also strengthen family bonds. Parents can encourage children to be more active by going on bike rides together. It’s a fun and healthy way to spend time as a family while developing good habits.
Stronger Muscles, Healthier Ageing
Cycling doesn’t just benefit your heart and lungs – it also strengthens muscles throughout your body, particularly in your legs, hips, and core. Each pedal stroke works your quadriceps, hamstrings, calves, and glutes. These muscle groups are essential for balance, walking, climbing stairs, and other daily activities.
As we age, maintaining muscle mass becomes increasingly important. Loss of muscle can lead to falls, injuries, and reduced independence. Cycling provides a low-impact, effective way to slow muscle loss and preserve strength, especially for older adults.
Indoor versus Outdoor: Which Ride Is Right for You?
One of the great things about cycling is that it can be done indoors or outdoors, each with its advantages.
Outdoor cycling is perfect for exploring new places, commuting, or getting on a longer endurance ride. It’s also a great social activity, whether you join a group ride or take a leisurely cruise with friends.
Indoor cycling, on the other hand, offers predictability and control. Whether you’re in a spin class or using a stationary bike at home, indoor cycling allows you to adjust intensity easily and stick to a consistent workout schedule, rain or shine.
For those with limited time or living in urban areas with traffic and safety concerns, indoor cycling may be a better option. Plus, many modern stationary bikes offer built-in workout programs, virtual classes, and tracking features to help keep you motivated.
Who Should Be Cautious About Cycling?
While cycling is safe for most people, there are a few exceptions. Individuals prone to falls or those with severe balance problems should avoid traditional outdoor biking. For these individuals, recumbent bikes are a great alternative. These bikes have a reclined seat and are lower to the ground, providing better stability and comfort. However, they can be more expensive and take up more space.
If you’re unsure whether cycling is right for you, talk to your healthcare provider, especially if you have chronic health conditions or are recovering from surgery.
How to Start and Stick With Cycling
Getting started is easier than you might think. All you need is a bike and a little motivation.
Start small: Begin with 10–15 minutes a day and gradually build up to longer rides.
Be consistent: Aim for 150 minutes per week. That’s just 30 minutes a day for five days.
Choose your style: Try different types of cycling – commuting, spin class, indoor biking, or scenic weekend rides.
Stay safe: Always wear a helmet, follow traffic rules, and use lights or reflectors if cycling outdoors at night.
If you’re cycling indoors, experiment with different virtual classes or programs to find what keeps you engaged. From high-energy spin sessions to scenic virtual rides, there’s something for everyone.
Final Thoughts: Just Keep Pedalling
Cycling is one of the most adaptable and rewarding exercises you can choose. It offers a long list of physical, mental, and lifestyle benefits – from reducing your risk of disease to saving money and improving the planet.
Whether you’re an athlete looking for a new challenge, a busy professional needing a flexible workout, or a senior aiming to stay active and mobile, cycling has something to offer you. So, grab a helmet, hop on a bike, and start pedalling your way to better health. The journey might just be your best ride yet.
Source: The Global New Light of Myanmar
Why is cycling one of the best Exercises for every lifestyle? In a world where people are becoming more aware of the importance of maintaining physical and mental health, finding the right form of exercise is key. For many, the solution might be simpler – and more enjoyable – than they think: cycling.
Whether you’re cruising down a quiet neighbourhood road, commuting to work, joining a spin class at the gym, or pedalling at home on a stationary bike, cycling is a powerful and flexible form of exercise. Not only does it improve physical health, but it also supports mental well-being, offers practical lifestyle benefits, and even helps protect the environment.
Let’s explore why cycling continues to gain popularity around the world and why it might just be the perfect activity to incorporate into your life – no matter your age, schedule, or fitness level.
An Exercise That Moves Your Heart (Literally)
One of the most celebrated benefits of cycling is how it supports heart health. As an aerobic exercise, cycling increases your heart rate and improves blood circulation throughout your body. Studies have shown that regular cyclists tend to have lower blood pressure and resting heart rates compared to inactive people.
Research has also revealed that people who cycle regularly are at a significantly reduced risk of developing coronary heart disease or suffering a heart attack. That’s because cycling helps keep your heart strong and arteries clear, reducing strain on the cardiovascular system. Just a few sessions a week, even at a moderate pace, can dramatically improve your cardiovascular fitness.
Gentle on the Joints, Powerful in Impact
Unlike activities such as running, which place repeated stress on your joints, cycling is a low-impact activity. This makes it especially appealing for people with joint issues, older adults, or those recovering from injuries.
Cycling is commonly used in physical therapy and rehabilitation programs. It promotes mobility, increases range of motion, and improves strength – all without putting your knees, hips, and ankles under heavy pressure.
A 2024 study found that people with osteoarthritis who incorporated cycling into their weekly routine experienced less knee pain than non-cyclists. This shows how effective and gentle cycling can be for long-term joint health.
Maintaining a Healthy Weight Made Easier
Weight management is a challenge for many, especially with busy schedules and sedentary lifestyles. Fortunately, cycling provides a fun, convenient way to help keep your weight in check. Regular cyclists often maintain a healthier body composition, which refers to the balance between fat, muscle, bone, and water in the body. Cycling burns calories, builds muscle, and boosts metabolism – all of which are essential for weight control.
The Centres for Disease Control and Prevention (CDC) recommends at least 150 minutes of moderate-intensity aerobic activity each week. Cycling is a great way to meet that recommendation. Whether you bike for 30 minutes five days a week or do three 50-minute sessions, you’ll be helping your body stay fit and active.
Want to lose weight? Increase your intensity by riding uphill, speeding up your pace, or extending your cycling sessions. These adjustments will boost your calorie burn and help you reach your goals faster.
Boost Your Mood, Beat the Blues
Exercise doesn’t just make your body stronger – it lifts your spirits, too. Physical activities like cycling release endorphins, the “feel-good” chemicals that improve mood and reduce stress.
People who cycle regularly often report better sleep, lower levels of anxiety and depression, and an overall improved sense of well-being. Whether it’s the rhythmic motion of pedalling or the calming effect of fresh air and sunshine, biking can be a great mental escape.
Cycling outdoors adds another layer of benefits. Being in nature, enjoying the scenery, and soaking in sunlight can help fight seasonal mood disorders and brighten your day, even after just a short ride.
Preventing Type 2 Diabetes Through Pedal Power
Cycling can play a key role in preventing chronic diseases such as type 2 diabetes. This condition is often linked to poor lifestyle habits, including a lack of physical activity and unhealthy weight gain. By promoting weight control and improving insulin sensitivity, cycling helps your body better regulate blood sugar levels. Studies have shown that people who bike to work or use cycling as a form of exercise have a significantly lower risk of developing type 2 diabetes.
Making cycling a part of your daily or weekly routine could be one of the simplest ways to protect your long-term health.
More Than Exercise: A Lifestyle Choice with Real-World Benefits
Cycling isn’t just a workout – it’s also a practical and sustainable way to live. When used as a mode of transportation, biking helps you save money on gas, parking, and public transport. It also reduces wear and tear on your vehicle and minimizes your carbon footprint. Each time you choose a bike over a car, you’re reducing greenhouse gas emissions. This is a powerful way to combat climate change and improve air quality in your community. Cleaner air leads to better public health and fewer respiratory issues, especially for children and the elderly.
Cycling can also strengthen family bonds. Parents can encourage children to be more active by going on bike rides together. It’s a fun and healthy way to spend time as a family while developing good habits.
Stronger Muscles, Healthier Ageing
Cycling doesn’t just benefit your heart and lungs – it also strengthens muscles throughout your body, particularly in your legs, hips, and core. Each pedal stroke works your quadriceps, hamstrings, calves, and glutes. These muscle groups are essential for balance, walking, climbing stairs, and other daily activities.
As we age, maintaining muscle mass becomes increasingly important. Loss of muscle can lead to falls, injuries, and reduced independence. Cycling provides a low-impact, effective way to slow muscle loss and preserve strength, especially for older adults.
Indoor versus Outdoor: Which Ride Is Right for You?
One of the great things about cycling is that it can be done indoors or outdoors, each with its advantages.
Outdoor cycling is perfect for exploring new places, commuting, or getting on a longer endurance ride. It’s also a great social activity, whether you join a group ride or take a leisurely cruise with friends.
Indoor cycling, on the other hand, offers predictability and control. Whether you’re in a spin class or using a stationary bike at home, indoor cycling allows you to adjust intensity easily and stick to a consistent workout schedule, rain or shine.
For those with limited time or living in urban areas with traffic and safety concerns, indoor cycling may be a better option. Plus, many modern stationary bikes offer built-in workout programs, virtual classes, and tracking features to help keep you motivated.
Who Should Be Cautious About Cycling?
While cycling is safe for most people, there are a few exceptions. Individuals prone to falls or those with severe balance problems should avoid traditional outdoor biking. For these individuals, recumbent bikes are a great alternative. These bikes have a reclined seat and are lower to the ground, providing better stability and comfort. However, they can be more expensive and take up more space.
If you’re unsure whether cycling is right for you, talk to your healthcare provider, especially if you have chronic health conditions or are recovering from surgery.
How to Start and Stick With Cycling
Getting started is easier than you might think. All you need is a bike and a little motivation.
Start small: Begin with 10–15 minutes a day and gradually build up to longer rides.
Be consistent: Aim for 150 minutes per week. That’s just 30 minutes a day for five days.
Choose your style: Try different types of cycling – commuting, spin class, indoor biking, or scenic weekend rides.
Stay safe: Always wear a helmet, follow traffic rules, and use lights or reflectors if cycling outdoors at night.
If you’re cycling indoors, experiment with different virtual classes or programs to find what keeps you engaged. From high-energy spin sessions to scenic virtual rides, there’s something for everyone.
Final Thoughts: Just Keep Pedalling
Cycling is one of the most adaptable and rewarding exercises you can choose. It offers a long list of physical, mental, and lifestyle benefits – from reducing your risk of disease to saving money and improving the planet.
Whether you’re an athlete looking for a new challenge, a busy professional needing a flexible workout, or a senior aiming to stay active and mobile, cycling has something to offer you. So, grab a helmet, hop on a bike, and start pedalling your way to better health. The journey might just be your best ride yet.
Source: The Global New Light of Myanmar